What Treatment Is Right For Me
The type of treatment will depend on how severe your symptoms are at the time of diagnosis with the goal being to control the disease to the point of remission and avoid complications. Medications may need to be changed over time to continue to maintain control and avoid disease progression and systemic effects. Some early indicators of more severe disease include onset at a young age, multiple joint involvement, and spinal involvement. Good control of the skin is important in the management of psoriatic arthritis. In many cases, you may be seen by two different types of healthcare providers, one in rheumatology and one in dermatology.
Early diagnosis and treatment can relieve pain and inflammation and help prevent progressive joint involvement and damage. Without treatment psoriatic arthritis can potentially be disabling, cause chronic pain, affect quality of life, and increase risk of heart disease. It is important to update your healthcare provider when you have a change in symptoms or if your medication regimen is no longer effective.
Similarities Between Psoriatic Arthritis And Psoriasis
Even though they are independent diseases, there are striking similarities between the two. Both the conditions are related, but it is not certain that a patient suffering from Psoriasis will develop Psoriatic arthritis. Acute inflammation is a common factor in both diseases. In both cases, the immune system attacks the body to cause this. Just like Psoriasis, the symptoms are not consistent. They can stay for months and then disappear only to come back after some time. Genetic factors, as well as environmental conditions, are responsible for both.
MEDICATION USED FOR TREATING BOTH PSORIATIC ARTHRITIS AND PSORIASIS
Although there is no permanent solution to these conditions, there are certain medicines that can help you to deal with the symptoms. is one such drug that is taken orally with or without food. It is usually started on a low dosage of 10 mg to see if the body is responding to it properly. Another kinase inhibitor named Tofacitinib is preferred by doctors to treat conditions where the body has not responded adequately to previous treatments. For treating moderate to severe Plaque Psoriasis, Etanercept is recommended by doctors. The usual dose is 25mg or 50mg twice a week, to which a number of patients have responded well. Tacrolimus is used to deal with Plaque Psoriasis, Inverse Psoriasis as well as refractory Psoriatic arthritis. It can be prescribed alone or in combination with other drugs.
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else. Psoriatic arthritis can be classed as a disability if its making every-day tasks difficult.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
You May Like: Can Psoriasis Be Detected By Blood Test
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
Recommended Reading: Can Rheumatoid Arthritis Affect Your Lungs
Understanding Psoriasis And Predisposition

While we know psoriasis is caused by the immune system, the exact cause is not known. The same can be said for psoriatic arthritis. Statistically, about 40 percent of people with psoriatic arthritis have relatives with psoriatic arthritis or with psoriasis, but scientists do not know what genes lead to these conditions. Ongoing research is investigating the causes of psoriasis and psoriatic arthritis in order to predict who may develop these conditions and to invent new treatments.
Read Also: Is Psoriasis Skin Disease Contagious
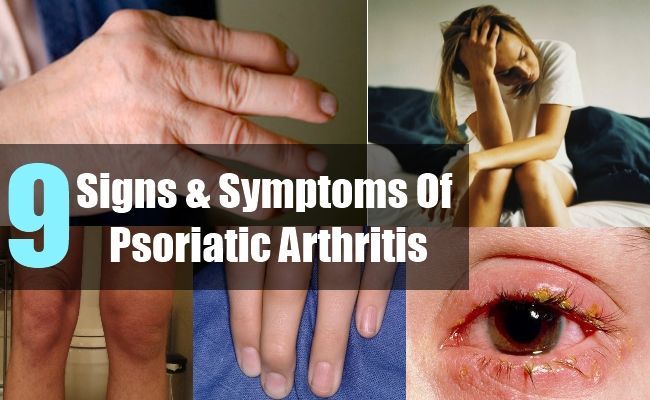
What Is Psoriatic Arthritis
This condition is mostly associated with joint inflammation that can also occur in combination with a skin disorder called Psoriasis. It can be difficult to distinguish this from other forms of arthritis because the symptoms are mostly the same. Maximum patients with this chronic inflammatory condition develop skin problems first. It can be categorized into the following:
- Distal Interphalangeal
- Swelling
Beautiful Acrylic Nails And Rheumatoid Arthritis For Natural Beauty
It is however possible to remove them yourself at home. The prevalence is estimated to be 1. acrylic nails and rheumatoid arthritis.
Acrylic Nails And Rheumatoid Arthritis, Lewis in his studies on the senile nail found thickening of the vessel walls in the nail generative areas and Sunderland and Ray 1952 have shown reduced nail growth following arterial ligation. Rheumatoid arthritis is a chronic inflammatory disorder. Acrylic Nails And Rheumatoid Arthritis.
Wear-and-tear arthritis also known as Osteoarthritis affects only one joint hand or finger arthritis but Rheumatoid arthritis affects both hands wrists ankles and fingers. Nail dystrophy in rheumatoid arthritis and it is interesting that there was a high incidence ofsuch changes in those patients who showed nail-edge or nail-fold vascular lesions. My nails are long and strong and I havent had a problem at all with them since RA diagnosisIn fact the girl who does my blood tests admired my nails a couple of months ago and she is now using the same and is very happy with her nails.
Recommended Reading: Cimzia Dosing For Plaque Psoriasis
What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
Are There Complications Of Psoriasis
In some people, psoriasis causes more than itchiness and red skin. It can lead to swollen joints and arthritis. If you have psoriasis, you may be at higher risk of:
- Use medicated shampoo for scales on your scalp.
Other steps you should take to stay as healthy as possible:
- Talk to your healthcare provider about lowering your risk for related conditions, such as heart disease, depression and diabetes.
- Lower your stress with meditation, exercise or seeing a mental health professional.
Read Also: Small Psoriasis Spots On Legs
When To Get Medical Advice
See a GP if you have persistent pain, swelling or stiffness in your joints even if you have not been diagnosed with psoriasis.
If you’ve been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let the doctor know if you’re experiencing any problems with your joints.
Treatment For Psoriatic Arthritis Differs From Other Forms Of Arthritis
The main goals of all arthritis treatment are to reduce symptoms and improve quality of life. Methods vary depending on the type of arthritis.
Rheumatoid arthritis can be very destructive if its not treated, which is why we treat it aggressively with biologics, says Ruderman. But psoriatic arthritis doesnt manifest that way. Fewer than half of people with psoriatic arthritis develop a particularly aggressive form, which makes treatment challenging because we dont want to over-treat it.
Even so, the pain and discomfort associated with psoriatic arthritis can be significant. A study published in 2015 in the journal PLoS One found that the overall pain, joint pain, and fatigue reported by psoriatic arthritis patients was significantly greater than that reported by people with rheumatoid arthritis.
Unless someone has an existing condition, such as elevated blood pressure or kidney disease, nonsteroidal anti-inflammatory drugs are recommended for joint symptoms in milder forms of psoriatic arthritis, says Husni.
Topical creams, ointments, and lotions are often used to address the scaly, itchy skin rashes that occur with psoriasis.
If there are signs of joint damage, doctors treat psoriatic arthritis more aggressively with medications like the ones used to treat rheumatoid arthritis, says Ruderman. These include disease-modifying anti-rheumatic drugs and biologics.
Additional reporting by Becky Upham.
Read Also: Dermatitis Or Psoriasis Of The Scalp
Underpinning Pathological Concepts For Common Ground Between Oa And Psa
It was proposed more than a decade ago that enthesitis may be the primary lesion in PsA and SpA . A number of imaging studies have since emerged showing that enthesopathy is common in psoriasis patients without clinical arthritis . Although it is difficult to prove the primacy of enthesitis in human PsA in all patients at all sites of disease, several animal models with features of PsA or SpA can clearly be shown to start at the enthesis . Likewise, several experimental studies have shown that spontaneous knee OA can start in the ligament and enthesis and not the articular cartilage, thus providing proof of principle of similar micro-anatomical topography for disease onset . Studies in the generalized form of human hand OA have also shown that the ligaments and enthesis are the sites of the earliest discernible pathology . The importance of the enthesis has also emerged in knee OA in man . Collectively this has resulted in a mechanistic anatomical classification of OA that recognizes that the generalized form of disease that was previously designated as idiopathic appears to have an enthesis-associated micro-anatomical basis .
The different entheses form what is now known as the synovialentheseal complex, where both degenerative and inflammatory processes can occur . If the pathological processes share the same micro-anatomical territory, then it is worth exploring anew the features that have been historically used to differentiate OA and PsA.
How Are Psoriasis And Psoriatic Arthritis Connected
You may have heard that psoriatic arthritis and psoriasis are connected, but might not understand how. Although the conditions share a similar name, they can have some very different symptoms and treatments. People with psoriasis are at a greater risk of developing psoriatic arthritis, and sometimes people with psoriatic arthritis develop psoriasis later on, meaning its helpful to have an understanding of both conditions if you are diagnosed with one, according to the Mayo Clinic.
Untangling the nuances between these two conditions can be a bit complicated. Thats why we spoke with experts about the important things you should know about psoriatic arthritis and psoriasis, including how the two are linked.
Also Check: Is Monggo Beans Bad For Arthritis
Also Check: Tea Tree Oil And Psoriasis
A Reappraisal Of Inflammation In Psa And Oa In Relation To Enthesopathy
While established PsA is an inflammatory arthropathy, evidence for inflammation in the preclinical disease phase may be absent. Evidence for a lack of association between inflammation and PsA is the presence of radiological sacroiliitis without concurrent clinical signs , which is also observed in subjects not known to have PsA . Degenerative changes at the SI joints can also mimic the appearance of inflammatory sacroiliitis, which causes a diagnostic challenge in identifying inflammatory low back pain . Moreover, imaging studies in psoriasis have consistently shown entheseal thickening without changes suggestive of inflammation, including a relative lack of Doppler enhancement on US . Asymptomatic areas of PsA also show thickening of the enthesis, suggesting a common site-specific tissue dysregulation as a precursor to disease . Furthermore, patients labelled as PsA who have normal CRP tend to have less responsiveness to anti-TNF therapy , suggesting the possibility of non-inflammatory pathways in pain in some of these cases, although this could also represent misdiagnosis of PsA, as discussed later.
How Are Ra And Psa Diagnosed
Because these two conditions share similar symptoms, it’s important to get an accurate diagnosis from a rheumatologist. A rheumatoid factor blood test is one way your doctor can tell which condition you have. RF is a protein found in people with rheumatoid arthritis. People with PsA usually don’t have it. Blood tests looking for other antibodies such as anti-CCP can also help differentiate the two.
Another way to tell is to look at your skin and nails. If you have scaly patches on your skin, pitting and flaking on your nails, or both, you have PsA.
Once you’ve had the disease for a while, X-rays might also be able to distinguish the two conditions.
It is possible to have RA and PsA together, but it’s rare. If you do have both, many of the treatments, including some medications, will work for both conditions.
Also Check: Does Psoriasis Itch And Burn
Clinical Implications Of Overlapping Features Of Oa And Psa
It may be genuinely difficult or even impossible to tell OA and PsA apart in a significant group of cases. Strategies including imaging may show erosion or periosteal new bone reaction in both, and MRI may not tell them apart . As an example of this, a recent study in subjects with psoriasis indicated the frequent occurrence of DISH, which is a degenerative disorder of the spine, which could very well have been ankylosis of the spine due to PsA . Furthermore, IA or local steroid injection may lead to some temporary relief in both OA and PsA or true overlaps. These findings are particularly important in the area of biologic therapy, where anti-TNF therapies are efficacious for PsA , but where there is no evidence that such therapies lead to significant symptomatic relief from OA . Nevertheless, in OA where there are clinically swollen joints, such strategies are associated with erosion progression retardation .
A study involving the Danish registry showed that failure to respond to anti-TNF therapy in PsA was associated with normal CRP as measured by conventional assays . Therefore it is possible that many failures of anti-TNF in PsA, at least in part, reflect the genuine inability of clinicians to differentiate OA from PsA. This may also be relevant for recent studies that have shown the apparent inefficacy of MTX in well-established PsA , whereas studies in early PsA patients who had a much greater elevation of CRP showed good evidence of efficacy .
Key Difference Plaque Psoriasis Vs Psoriasis
Psoriasis is one of the most common dermatological problems that can have adverse effects on both social and mental well-being of the patient. It is an autoimmune condition whose pathogenesis is triggered by different intrinsic and extrinsic factors. Psoriasis can be defined as a chronic multisystem disease with skin and joint manifestations. There are different forms of psoriasis including guttate psoriasis, pustular psoriasis, etc. Out of them, plaque psoriasis is the commonest form of psoriasis which is characterized by the appearance of reddish well-demarcated plaques with silver scales usually on the extensor surface of the knees and elbows. So plaque psoriasis is one element of psoriasis which can have various other clinical manifestations. This is the key difference between Plaque Psoriasis and Psoriasis.
Also Check: Where To Buy Imak Arthritis Gloves
Don’t Miss: Is Eucrisa Used For Psoriasis