Psoriasis And Celiac Disease
When you have celiac disease, you can’t digest gluten, a protein in wheat, rye, and barley. Celiac disease can damage your small intestine and prevent it from absorbing key nutrients.
The chance of getting celiac disease is nearly 3 times higher among people with psoriasis. About 4 of every 100 have it. Research shows that the higher the levels of specific antibodies related to celiac disease, the worse psoriasis tends to be.
A Common Inflammatory Pathway
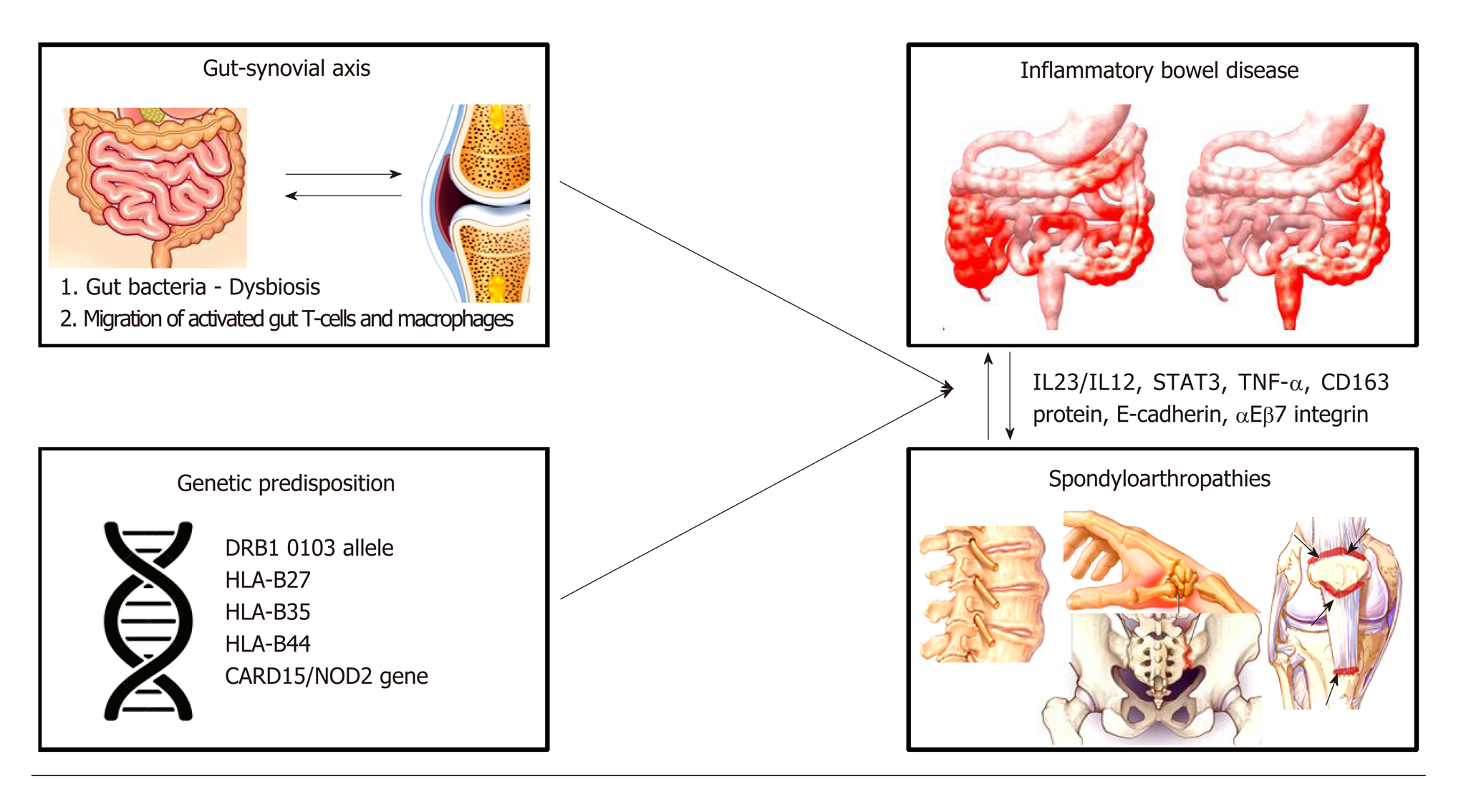
As researchers discover more about the inflammatory pathways of IBD and psoriasis, some overlap between the two diseases is being uncovered . Crohn’s disease and psoriasis are both considered Th1 mediated conditions. Th1 is a helper cell that mounts an inflammatory response when the body is invaded by a foreign substance such as a parasite, bacteria, or virus. Ulcerative colitis is considered a Th2-like mediated condition. Th2 cells are activated when there is a bacteria, allergic response, or toxin present. As the role of these T cells is better understood in regards to the development of IBD and psoriasis, it could lead to the creation of more effective treatments for these diseases.
Risk Factors For Developing Psoriasis
Both psoriasis and CD have genetic risk factors and are linked to an increased prevalence of each of these conditions among first-degree family members parents, children, and siblings. Some other risk factors for developing psoriasis, with or without IBD, include:
- Obesity
- Some viral and bacterial infections
Recommended Reading: Mg217 Psoriasis Multi Symptom Moisturizing Cream
Comparison Of Pharmacologic Treatment Modalities
The wide overlap of approved modalities employed to treat psoriasis and IBD, particularly the more targeted newer biologics, underscore the pathophysiologic proximity of the mechanisms that underlie the pathogenesis of these conditions. However, distinct differences also exist that obviate core differences in the pathophysiology of these conditions, and the knowledge of these differences is significant for the understanding of core pathomechanistic peculiarities of each condition. depicts and compares the use of currently approved pharmacologic modalities for the systematic treatment of psoriasis and IBD.
Risk Of Bias And Quality Assessment
Outliers were identified with externally standardized residuals in R version 3.6.1 . Absolute values of Z-scores greater than or equal to two were identified as outliers. Influential studies were identified as those with a Cooks distance larger than three times the mean value. Studies that were outliers and influential were assessed for quality with the Newcastle-Ottawa Scale . The tool includes three domains: selection, comparability, and outcome/exposure. The threshold for good quality was a minimum of 3 stars in the selection domain and 1 star in the comparability domain and 2 stars in the outcome/exposure domain. Influential outliers that were good quality according to the NOS were included in the study.
Recommended Reading: Why Is My Psoriasis Coming Back
Crohns Disease Psoriasis And Psoriatic Arthritis: Whats The Connection
Psoriasis and psoriatic arthritis are linked to Crohns disease and ulcerative colitis , and either condition may be a comorbidity for some people with psoriasis. A comorbidity is when two or more disorders occur in the same person and cause adverse interactions.
CD and UC are forms of inflammatory bowel disease . CD causes chronic inflammation in the lining and deeper layers of the digestive tract. UC is characterized by inflammation and sores in the lining of the large intestine and rectum.
Psoriasis causes an overproduction of skin cells that become dry, itchy, and discolored patches of thick, scaly skin lesions , which can become infected during flares. Approximately 30 percent of people with psoriasis develop PsA with symptoms such as tendon pain, joint pain, swollen and stiff joints, fatigue, and eye redness and pain .
For people with psoriasis, the increased risk for UC is approximately 1.6 times greater than the general population. The risk for CD is about 2.5 times higher than average.
MyPsoriasisTeam members have shared their experiences with psoriasis, PsA, and CD. I was diagnosed with Crohns last October, having been really sick all year, said a member. One good thing if there is one about having Crohns is that my psoriasis has gotten a lot better, she added.
Does anyone else suffer from Crohns and psoriatic arthritis , but I dont know anyone else with both conditions, wrote another member.
Medical Treatment For Uc
Table 3. Evidence from clinical trials for class of therapeutic options for ulcerative colitis.
Due to the ineffectiveness of IL-17i for CD, there have not been trials for their use in UC. As for IL-23i, there is an ongoing phase II/III trial of RZB for UC .
In contrast to CD, the JAKi, TOF, was approved for use in moderate-to-severe UC based on three pivotal phase III OCTAVE studies, showing a significantly greater percentage of clinical remission at week 8 for induction, and remission at week 52 for maintenance in TOF compared to placebo group . UPA met the clinical remission, endoscopic improvement and histological improvement endpoints in a phase III induction trial for moderate-to-severe UC .
Recommended Reading: Hydrocortisone For Psoriasis On Face
Psoriasis Linked To Increased Risk For Crohns Ulcerative Colitis
We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Patients with psoriasis are increasingly linked to risks for Crohns disease, ulcerative colitis and a combination of the two diseases, according to a review study published in JAMA Dermatology.
We found that patients with psoriasis were prone to have comorbid IBD,Yen Fu, MD, and colleagues wrote. The possible explanations for the identified association of psoriasis with IBD include genetic abnormalities, immune dysfunction, systemic inflammation, and dysregulation of gut microbiota.
Fu and colleagues analyzed five case-control or cross-sectional studies and four cohort studies, totaling 7,794,087 study participants. The systematic review and meta-analysis included relevant studies through January 17, 2018.
They found associations between psoriasis and CD and between psoriasis and UC . When psoriasis was present, patients had an increased risk for CD and UC .
Additionally, the researchers looked at participants with psoriatic arthritis and, through the meta-analysis, found a significantly increased risk for CD and a nonsignificant increase in the risk for UC in patients with psoriatic arthritis.
Disclosures: The researchers report no relevant financial disclosures.
Link Between Psoriasis And Inflammatory Bowel Disease
What is inflammatory bowel disease? IBD can include Crohns disease and ulcerative colitis. Learn more about testing, treatments, and the home care needed to manage IBD. home digestive disorders center digestive disorders a-z list slideshow.
Rationale and background: Inflammatory bowel disease has been reported to frequently co-occur in patients with manifest psoriasis and psoriatic.
Epidermolysis bullosa acquisita and inflammatory bowel disease. JAMA 1983 250:1746. Najarian DJ, Gottlieb AB. Connections between psoriasis and.
To evaluate the association of psoriasis and PsA with IBD and other GI illnesses, the researchers identified data from the National.
Psoriasis and the spectrum of inflammatory bowel diseases are chronic, inflammatory, organotropic conditions. The epidemiologic coexistence of these diseases is corroborated by findings at.
Results: Prevalence of inflammatory bowel disease, Crohn’s disease and ulcerative colitis in patients with psoriasis vs the general population in 2011 were 0.16, 0.05 and 0.12% vs 0.08, 0.03 and 0.
Psoriasis and the spectrum of inflammatory bowel diseases are chronic, inflammatory, organotropic conditions. The epidemiologic coexistence of these diseases is corroborated by findings at.
Background: The epidemiology of the association between psoriasis and inflammatory bowel disease is poorly defined and remains controversial.
studies showing there may be equipoise between chemoradiation and surgery and chemo.
Also Check: Does Scalp Psoriasis Smell Bad
The Connection Between Ibd And Psoriasis
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
People who have inflammatory bowel disease also sometimes develop other diseases or conditions that are called extra-intestinal manifestations . Skin conditions are fairly common in people with IBD, and one that tends to occur frequently both in the general population and in people with IBD is psoriasis. Many people may think of psoriasis as a rash, but it’s actually a systemic condition and may share the same inflammatory pathway as Crohn’s disease. Because the two conditions might be caused by a problem in the functioning of the immune system, they are often treated by some of the same medications. For people with IBD who also have psoriasis, both conditions may be a factor when choosing treatments.
There are a variety of effective treatments for psoriasis already available and more are currently being developed. People who have both psoriasis and IBD will want to seek care from a dermatologist that has experience with patients with IBD and will work closely with the gastroenterologist.
Biologic Treatment Psoriasis And Ibd
Biologic drugs are used in the treatment of IBD and psoriasis to target cytokines proinflammatory proteins in the immune system that are associated with psoriasis and IBD.
Tumor necrosis factor – inhibitors , interleukin -23 inhibitors, IL-12 inhibitors, and integrin receptor antagonists are biologic therapies used in the treatment of Crohns and UC. IBD and psoriasis share some of the same immune system pathways, and both diseases may be treated together with biologic drugs when they occur at the same time.
However, research has shown that treatment of psoriasis with IL-17 inhibitors has a risk of inducing or exacerbating IBD in some people. IL-17 inhibitors aggravate inflammation in some individuals with CD in particular and are a risk factor for developing the condition. IL-17 inhibitors have also been linked with a risk of moderately exacerbating UC.
IL-17 inhibitors used in the treatment of psoriasis include:
- Taltz
- Cosentyx
- Siliq
Certain biologic drugs can effectively treat some people who have both IBD and psoriasis without the added risk of triggering Crohns or UC. Those biologics include:
Recommended Reading: Apple Cider Vinegar For Plaque Psoriasis
Medical Treatment For Uveitis
Table 4. Evidence from clinical trials for class of therapeutic options for uveitis.
Despite implicated in the pathogenesis of uveitis, inhibiting IL-17A was not effective for uveitis. In three RCTs, SEC failed to meet the primary efficacy endpoints . In another RCT comparing three doses of SEC, statistical higher response rates and remission on day 57 for the high dose regimen was seen compared to the other two lower dose regimens, suggesting a higher dose intravenous regimen may be required to deliver SEC in therapeutic concentrations . Results are awaiting for two trials using UST in active sight-threatening uveitis and Behçet uveitis , which may provide insight for its potential use in PsA related uveitis.
Minimal data exist for use of JAKi in uveitis. One phase 2 RCT evaluating filgotinib in patients with active non-infectious uveitis is ongoing.
How Is Ibd Treated
Neither psoriasis nor IBD has a cure, but both can be treated and many people find that they are able to manage their symptoms. The aim of treating IBD is to reduce the amount of inflammation in the persons digestive tract, which helps to improve symptoms and prevent further damage1. For people with milder forms of IBD, anti-inflammatory medicines called aminosalicylates are often recommended.
Several of the same medications that are used to treat more severe psoriasis are also used to treat moderate or severe inflammatory bowel disease. These are powerful drugs that work by reducing the amount of inflammation in the entire body, such as:
- Systemic medicines, such as methotrexate
- Biologic therapies, such as infliximab and adalimumab
Around 75% of patients with Crohns disease and 25% patients with ulcerative colitis will eventually need to have surgery to treat the condition2. The type of procedure needed can vary, from surgery to widening areas of the intestine that have become too narrow to procedures to remove small or large sections of the intestine.
Don’t Miss: Laser Light Treatment For Psoriasis
Topical And Light Therapy Treatments For Psoriasis
There are several treatments for psoriasis, including light therapy, topical treatments, and medications. In many cases, more than one treatment might be used at the same time to combat the symptoms of psoriasis. Generally, topical therapies might be tried first, before moving on to light therapy or systemic medications.
- Topical treatments. There are various types of creams and ointments that may be used for psoriasis, both over the counter and prescription. Some of the active ingredients include corticosteroids, vitamin D, retinoids, anthralin, calcineurin inhibitors , salicylic acid, and coal tar. In some cases, moisturizers might also be used to combat dryness.
- Light therapy. Light that contains ultraviolet A and ultraviolet B may also be used to treat psoriasis. This is usually used along with other treatments. Sunlight from outside might be used, for short periods of time. Ultraviolet rays can also be administered via phototherapy with a light panel, box, or booth. In severe cases, a medication that makes the skin more sensitive to ultraviolet light might also be used at the same time as light therapy in order to make it more effective. A type of laser is also sometimes used because it can target specific areas on the body with a stronger dose of ultraviolet B light.
Management Of Psa With Consideration Of Extra
Given the heterogeneity in manifestations, enhanced collaboration between disciplines are required to deliver optimal care for PsD . While collaborations between rheumatologists and dermatologists are increasing , collaborations with gastroenterologists and ophthalmologists have traditionally been weaker. Apart from setting up combined clinics, collaborations between disciplines can take other forms as determined by needs and circumstances of different institutions. Minimally, identifying key stakeholders specializing in the care of PsA patients and keeping them in close communication over the management plan is essential. These collaborations serve both clinical and educational needs. Close collaboration between the various disciplines will help in early diagnosis of the various manifestations, providing expert advice on choice of therapeutics to create a patient-centric, individualized care plan for the heterogeneous manifestations. Often, the therapeutics will need to cover multiple domains, but the predominant domain should drive the therapeutic option of choice in the shared decision-making process.
All in all, detailed considerations of all domains and extra-articular manifestations are necessary to formulate the best therapeutic option. Multi-disciplinary collaborative care models are advocated for optimal care for patients with PsA, and especially so for those who present with co-morbidities.
Also Check: Early Signs Of Psoriasis On Scalp
Risk Factors For Developing Ibd
Both psoriasis and CD are associated with an increased prevalence of these conditions among first-degree family members, which include parents, children, and siblings. Some of the environmental factors for developing either type of IBD, with or without psoriasis, include:
- Birth by cesarean section
- City air pollution
- Dysbiosis
Oral contraceptives, antibiotics, and nonsteroidal anti-inflammatory drugs other than aspirin are also associated with a higher incidence of developing IBD.
Managing Psoriatic Arthritis With Inflammatory Bowel Disease And/or Uveitis
- 1Duke-NUS Medical School, Singapore, Singapore
- 2Translational Immunology Institute, SingHealth Duke-NUS Academic Medical Centre, Duke-NUS Medical School, Singapore, Singapore
- 3Singapore National Eye Center and Singapore Eye Research Center, Singapore, Singapore
- 4Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore, Singapore
- 5Department of Rheumatology and Immunology, Singapore General Hospital, Singapore, Singapore
Psoriatic arthritis is a chronic inflammatory disease that presents with psoriasis , peripheral and axial arthropathy. The heterogeneity of disease presentation leads to the term psoriatic disease which is thought to better encompass the range of clinical manifestations. PsA is associated with several comorbidities such as cardiovascular diseases, metabolic syndrome and other extra-articular manifestations including uveitis, and inflammatory bowel disease . While novel therapeutics are being developed following advances in our understanding of the pathogenesis of the disease, the diverse combinations of PsA with its various comorbidities still pose a clinical challenge in managing patients with PsA. This article reviews our current understanding of the pathogenesis of PsA and how various pathways in the pathogenesis lead to the two comorbid extra-articular manifestations uveitis and IBD. We also review current evidence of treatment strategies in managing patients with PsA with comorbidities of uveitis and/or IBD.
Don’t Miss: Is Eucrisa Good For Psoriasis
Treating Concurrent Psoriasis And Ibd: Which Options Are Best
The biologics infliximab and adalimumab are safe and effective for the treatment of psoriasis, psoriatic arthritis , ulcerative colitis , and Crohn disease in patients with inflammatory bowel disease , a recent study found.
For their study, the researchers first performed a systematic literature search and identified 2282 articles that had studied biologic and systemic psoriasis medications in psoriasis, PsA, UC, and CD between January 1, 1947 and February 14, 2017. Of these articles, 132 were included in the present analysis._____________________________________________________________________________
FDA Expands Psoriasis Drug’s Indication_____________________________________________________________________________
Findings showed that infliximab and adalimumab were safe and effective for the treatment of psoriasis, PsA, UC, and CD. However, none of the other treatments assessed could be used for the treatment of all 4 of these conditions. Ustekinumab could be used to treat psoriasis, PsA, and CD, while certolizumab could only be used to treat PsA and CD.
Guselkumab was also found to effectively treat psoriasis. The researchers noted that, although psoriasis and PsA can be successfully treated with etanercept, secukinumab, brodalumab, and ixekizumab, they may worsen or induce IBD.
Christina Vogt
Reference:
What Are The Causes And Symptoms Of Ibd
The exact causes of IBD are still unknown. However, researchers think that they are probably caused by a combination of genetics, the environment, and microorganisms in the gut . The current theory is that these diseases develop when a persons immune system has the genetic tendency to overreact to harmless microorganisms in the gut1. This reaction causes chronic inflammation anywhere along the digestive tract. The differences between Crohns disease and ulcerative colitis have to do with the location and severity of the symptoms2.
Recommended Reading: Common Places To Get Psoriasis