Symptoms Of Psoriatic Arthritis
The severity of the condition can vary considerably from person to person. Some people may have severe problems affecting many joints, whereas others may only notice mild symptoms in 1 or 2 joints.
There may be times when your symptoms improve and periods when they get worse .
Relapses can be very difficult to predict, but can often be managed with medicine when they do occur.
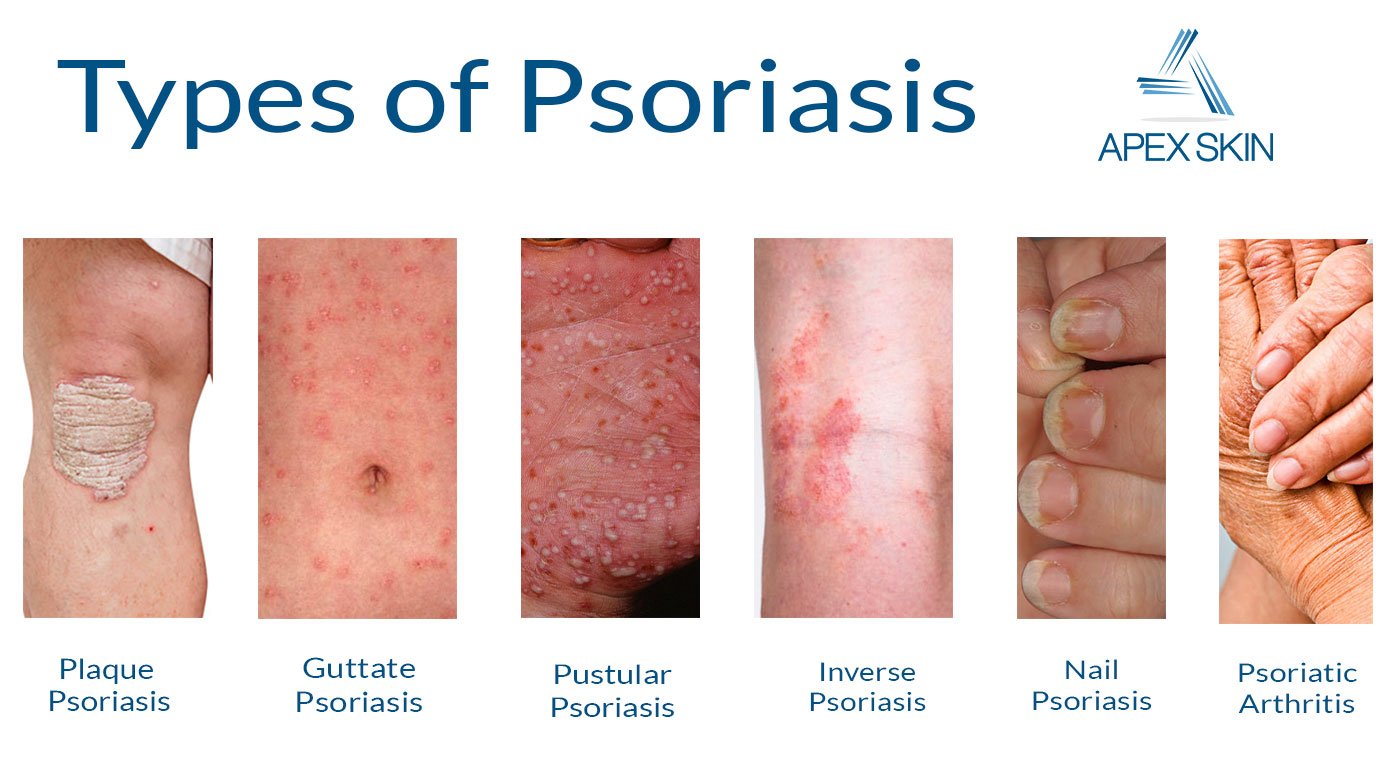
What Are The Symptoms Of Psoriasis
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Where They Show Up
Eczema often appears on parts of your body that bend, like your inner elbow or behind your knees. You can have it on your neck, wrists, and ankles. Babies sometimes get it on their chin, cheeks, scalp, chest, back, arms, and legs.
Psoriasis often shows up on places like your:
- Elbows
- Dandruff
- Some foods
Infections can start up eczema, and so can stress, sweating, heat, humidity, and changes in your hormones.
Psoriasis shares some of these triggers, like stress and infection. But you can also get flare-ups when your skin is injured, for example by:
- Vaccination
- Sunburn
- Scratches
Some medications can also bring on a psoriasis flare, like lithium, which treats bipolar disorder, or drugs for malaria.
You May Like: How Long Does Stelara Take To Work For Psoriasis
Imaging Tests For Psa And Ra
Imaging tests, such as X-rays and magnetic resonance imaging , are useful in diagnosing both PsA and RA, as well as learning how far the disease has advanced.
X-rays are the first line of diagnosis for both conditions, as they are inexpensive and easy to reproduce. More sensitive technologies, like MRI, are costlier and are therefore used as second-line diagnostic tools.
PsA and RA can produce different patterns of inflammation on imaging scans, and ultrasound can be useful in detecting these patterns and getting a definitive diagnosis.
Who Will Be Responsible For My Healthcare
Youre likely to see a team of healthcare professionals.
Your doctor, usually a rheumatologist, will be responsible for your overall care. And a specialist nurse may help monitor your condition and treatments. A skin specialist called a dermatologist may be responsible for the treatment of your psoriasis.
You may also see:
- a physiotherapist, who can advise on exercises to help maintain your mobility
- an occupational therapist, who can help you protect your joints, for example, by using splints for the wrist or knee braces. You may be advised to change the way you do some tasks to reduce the strain on your joints.
- a podiatrist, who can assess your footcare needs and offer advice on special insoles and good supportive footwear.
Don’t Miss: New Drug For Psoriasis 2017
Articles On Psoriasis Symptoms
Maybe you’re settling into your easy chair for a little Sunday siesta. Or you’re heading out the door for a day of fun in the sun. Either way, you stop and pause, because you’ve got an itch that just won’t leave you alone — along with blotches of red on your skin. What gives?
Your doctor needs to make the final call, but psoriasis or eczema could be the problem. Both are skin conditions with similar symptoms, but there are ways to tell them apart.
What Treatment Is Right For Me
The type of treatment will depend on how severe your symptoms are at the time of diagnosis with the goal being to control the disease to the point of remission and avoid complications. Medications may need to be changed over time to continue to maintain control and avoid disease progression and systemic effects. Some early indicators of more severe disease include onset at a young age, multiple joint involvement, and spinal involvement. Good control of the skin is important in the management of psoriatic arthritis. In many cases, you may be seen by two different types of healthcare providers, one in rheumatology and one in dermatology.
Early diagnosis and treatment can relieve pain and inflammation and help prevent progressive joint involvement and damage. Without treatment psoriatic arthritis can potentially be disabling, cause chronic pain, affect quality of life, and increase risk of heart disease. It is important to update your healthcare provider when you have a change in symptoms or if your medication regimen is no longer effective.
Also Check: How To Tell If You Have Psoriasis
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
Efficacy Of Mtx In Psoriasis And Psa
To open the debate on MTX use, S.M. Grieb discussed personal experiences from the GRAPPA PRP. Prior to the 2019 GRAPPA annual meeting, PRP were asked to respond to questions regarding their personal experience using MTX. Of the PRP, 11 of 13 responded, with 10 sharing their experiences, and 1 indicating no MTX use. Of those with experience using MTX, the majority used the tablet form, sometimes as monotherapy and sometimes in conjunction with additional medicines. Only 3 PRP had experience with the injectable form. Most of the PRP indicated that MTX did little to help their disease. The benefits they experienced were largely in the skin, while there was only a limited effect reported on arthritis. For the 3 PRP who responded well to the medication, the effect on their health and well-being was great. One PRP stated, At first it was a revelation. Relatively quickly I was relieved of the feeling that I was moving my body through the weight of deep water, and movement became easier again, less painful. The psoriasis relief followed. However, for 2 of the 3 who found relief using MTX, it was unfortunately not sustained.
Read Also: How To Get Psoriasis Out Of Ears
Survey: The Current And Future Role Of Mtx
Following the presentations, a final audience survey was held to gather opinions on MTXs current and predicted future roles in clinical practice. Given the recent ACR recommendation to use TNFi first before oral small molecules for PsA, the audience was asked, If cost were no object, would you use TNFi first line for PsA? A total of 69% answered yes, with rheumatologists and dermatologists responding similarly. There was variation in responses by geographical region, with first-line use of TNFi supported by 76% of Europeans, 88% of North Americans, but only 37% of South Americans.
The audience was then asked, If cost were no object, which treatment would you use first line for moderate/severe plaque psoriasis? Here, the majority voted for either interleukin -17 inhibitors or IL-23 inhibitors , with 14% supporting the use of MTX. In this case, dermatologists and rheumatologists differed, with dermatologists choosing IL-17 and IL-23 inhibitors in identical proportions , and rheumatologists choosing IL-17 over IL-23 inhibitors , possibly because rheumatologists have a limited familiarity with IL-23 inhibitors. Again, there was some variation by geographical region IL-23 inhibitors were the most popular North American choice , with IL-17 inhibitors as the most popular European and South American choice. MTX was chosen by 19% of South American participants, 12% of European participants, and only 5% of North American participants.
The Differences In Appearances
Eczema makes your skin red and inflamed. It may be scaly, oozing, or crusty. You may see rough, leathery patches that are sometimes dark. It can also cause swelling.
Psoriasis can also cause red patches. They may be silvery and scaly — and raised. But if you look closely, the skin is thicker and more inflamed than with eczema.
Read Also: Difference Between Psoriasis And Dermatitis
Psoriatic Arthritis Treatment Options
Psoriatic arthritis symptoms can be treated with systemic drugs that affect your whole body. Depending on your unique case of psoriatic arthritis, your dermatologist may prescribe methotrexate, cyclosporine or certain biologics. In some cases, steroid injections can reduce inflammation quickly in an affected joint. At Dermatology Associates of Plymouth Meeting, we may team with a board-certified rheumatologist to treat joint disease linked to psoriatic arthritis.
In addition to these medications or treatment options, whether you are experiencing psoriasis or psoriatic arthritis, your dermatologist may recommend lifestyle changes to help minimize symptoms and flare ups. We always encourage changes such as quitting smoking, drinking less and minimizing stressors which can help with psoriasis and psoriatic arthritis flare ups. With psoriasis and psoriatic arthritis, it is common for symptoms to come and go, but it is important to continue taking medication and undergoing treatments recommended by your dermatologist.
If you are struggling to manage your plaque psoriasis or psoriatic arthritis, schedule an appointment today. Our team of board-certified dermatologists are experts in treating all types of psoriasis and can develop a personalized treatment plan based on your unique background and needs.
Recent Posts
How Are Ra And Psa Diagnosed
Because these two conditions share similar symptoms, itâs important to get an accurate diagnosis from a rheumatologist. A rheumatoid factor blood test is one way your doctor can tell which condition you have. RF is a protein found in people with rheumatoid arthritis. People with PsA usually donât have it. Blood tests looking for other antibodies such as anti-CCP can also help differentiate the two.
Another way to tell is to look at your skin and nails. If you have scaly patches on your skin, pitting and flaking on your nails, or both, you have PsA.
Once youâve had the disease for a while, X-rays might also be able to distinguish the two conditions.
It is possible to have RA and PsA together, but itâs rare. If you do have both, many of the treatments, including some medications, will work for both conditions.
Also Check: Does Psoriasis Itch And Burn
Also Check: Best Lotion For Psoriasis On Face
Treatment For Psoriatic Arthritis Differs From Other Forms Of Arthritis
The main goals of all arthritis treatment are to reduce symptoms and improve quality of life. Methods vary depending on the type of arthritis.
Rheumatoid arthritis can be very destructive if its not treated, which is why we treat it aggressively with biologics, says Ruderman. But psoriatic arthritis doesnt manifest that way. Fewer than half of people with psoriatic arthritis develop a particularly aggressive form, which makes treatment challenging because we dont want to over-treat it.
Even so, the pain and discomfort associated with psoriatic arthritis can be significant. A study published in 2015 in the journal PLoS One found that the overall pain, joint pain, and fatigue reported by psoriatic arthritis patients was significantly greater than that reported by people with rheumatoid arthritis.
Unless someone has an existing condition, such as elevated blood pressure or kidney disease, nonsteroidal anti-inflammatory drugs are recommended for joint symptoms in milder forms of psoriatic arthritis, says Husni.
Topical creams, ointments, and lotions are often used to address the scaly, itchy skin rashes that occur with psoriasis.
Read Also: Dermatitis Or Psoriasis Of The Scalp
Beautiful Acrylic Nails And Rheumatoid Arthritis For Natural Beauty
It is however possible to remove them yourself at home. The prevalence is estimated to be 1. acrylic nails and rheumatoid arthritis.
Acrylic Nails And Rheumatoid Arthritis, Lewis in his studies on the senile nail found thickening of the vessel walls in the nail generative areas and Sunderland and Ray 1952 have shown reduced nail growth following arterial ligation. Rheumatoid arthritis is a chronic inflammatory disorder. Acrylic Nails And Rheumatoid Arthritis.
Wear-and-tear arthritis also known as Osteoarthritis affects only one joint hand or finger arthritis but Rheumatoid arthritis affects both hands wrists ankles and fingers. Nail dystrophy in rheumatoid arthritis and it is interesting that there was a high incidence ofsuch changes in those patients who showed nail-edge or nail-fold vascular lesions. My nails are long and strong and I havent had a problem at all with them since RA diagnosisIn fact the girl who does my blood tests admired my nails a couple of months ago and she is now using the same and is very happy with her nails.
Read Also: What Causes Psoriasis In Children
Patient Demographics And Diagnosis History
Of > 265 million patients in the MarketScan databases, 280,311 patients had 1 diagnosis of PsA and 174,524 patients had 2 diagnoses of PsA 30 days apart, of whom 172,119 patients were aged 18 years at the index date. Of these, a final cohort of 13,661 patients had 6 years of continuous enrolment in the database, fulfilling the criteria for inclusion in the study. The mean age was 55.8 years and 60.2% were women baseline demographics of patients diagnosed with PsA and non-PsA controls are shown in Table .
Table 1 Baseline demographics of patients diagnosed with PsA and non-PsA controls
Psoriatic Arthritis Documentation Related Icd
According to the National Psoriasis Foundation, up to 30% of people with psoriasis develop psoriatic arthritis , an inflammatory form of arthritis. It can also occur in people without the skin symptoms of psoriasis. This chronic inflammatory arthritis associated with psoriasis can also be confused with osteoarthritis , the most common form of arthritis. This highly heterogeneous disorder can affect multiple different tissues, including the peripheral joints, skin, axial joints, enthesitis and dactylitis . As the condition is easy to confuse with other diseases, specialists in musculoskeletal disorders, and rheumatologists are more likely to make a proper diagnosis and advise patients about the best treatment options. Outsourcing medical billing tasks will help these specialists reduce documentation work and focus on patient care.
Typical symptoms are fatigue, nail changes and reduced range of motion of affected joints. PsA can affect any joint in any pattern, and may affect one joint at a time, to start with. Patients are also at the risk of developing further complications such as
- arthritis mutilans which destroys the small bones in the hands
- eye problems such as conjunctivitis, uveitis, and an increased risk of cataracts and glaucoma
- co-morbid conditions stroke, cardiovascular problems, depression, diabetes mellitus type 2, lymphoma, skin cancer, osteoporosis , and hearing loss
- L40 Psoriasis
You May Like: Is The Tanning Bed Good For Psoriasis
Add Exercise To Your Daily Routine If You Can
Keeping your joints moving can ease stiffness. Being active for at least 30 minutes per day will also help you lose excess weight and give you more energy. Ask your doctor what type of exercise is safest for your joints.
Biking, walking, swimming, and other water exercises are gentler on the joints than high-impact exercises like running or playing tennis.
Classification Of Psoriatic Arthritis
Psoriatic arthritis is a form of spondyloarthritis. Spondyloarthritis is an umbrella term used to describe a family of disorders, including ankylosing spondylitis, non-radiographic axial spondyloarthritis, psoriatic arthritis, reactive arthritis, enteropathic arthritis and undifferentiated spondyloarthritis. These different forms of spondyloarthritis share several clinical features:
- Axial joint inflammation
- Asymmetric oligoarthritis
- Dactylitis: ‘sausage digits’
- Enthesitis: pain and swelling at the insertion of tendons and ligaments, commonly at the heel, tibial tuberosity and humerus this affects up to 53% of patients with psoriatic arthritis
- Negative Rheumatoid Factor
- HLA-B27 positivity: HLA-B27 is a specific protein involved with immune regulation. 57% of psoriatic arthritis patients with axial involvement are positive for HLA-B27
- Geneticsusceptibility to the condition/family history
- Distinctive radiological features.
You May Like: What Is Good For Eczema And Psoriasis
Psoriatic Arthritis Signs And Symptoms
Early symptoms with psoriatic arthritis are important. People will complain of pain and swelling in their joints hands, feet, wrists, etc. They may have a small patch of psoriasis or have psoriasis covering many areas of the body. There may be complaints of stiffness and fatigue. For example, studies in Toronto showed the year before they were diagnosed, people had reported joint pain, fatigue, and stiffness. Early in the disease, people will often have episodes of worsening of the psoriatic arthritis and then episodes of improvement.
What Causes Psoriasis And Psoriatic Arthritis
The symptoms of both psoriasis and psoriatic arthritis arise when the bodys immune system malfunctions, leading to inflammation.
In psoriasis, the faulty reaction causes skin cells to grow too fast, promoting a buildup of skin cells on the surface. These cells appear as a scaly rash.
In psoriatic arthritis, the inflammation affects the joints. Permanent damage can result if the person does not seek treatment.
Doctors do not yet know the exact causes of psoriasis and psoriatic arthritis. However, they do know that genetics contribute to both conditions.
An estimated 1 out of 3 people with psoriasis say that they have a family member with psoriasis. Also, around 40 percent of people with psoriatic arthritis have a family member with psoriatic disease.
Still, many people have genes for psoriatic disease and never develop it. To develop psoriatic disease, a person must have the specific genes for it, as well as a trigger that activates it.
Possible triggers for psoriatic disease include:
- an infection, such as strep throat or a cold
- use of tobacco or smoking
- heavy alcohol use
These triggers may bring on psoriasis, and they can also cause flares. Flares are cycles during which symptoms become worse. Triggers vary from person to person and may change over time.
Psoriasis and psoriatic arthritis symptoms often come and go in cycles. They may get worse during a flare and then improve. Symptoms may also move around, affecting different areas of the body at different times.
Recommended Reading: What Is Autoimmune Disease Psoriasis