What Is The Evidence That Psoriasis Has An Autoimmune Component
Some forms of psoriasis show strong associations with autoimmunity. For example, there is a rare type of psoriasis called pustular psoriasis in which patients develop sterile pustules on top of red plaques . The association between this form of psoriasis and autoimmunity was recognized as early as 1908 . More recently, research has demonstrated that patients with pustular psoriasis often have positive tests for antibodies against the cells lining blood vessels , called endothelium-specific autoantibodies .
Having Psoriasis During The Covid
Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
This has been reviewed and updated as of May 29, 2020.
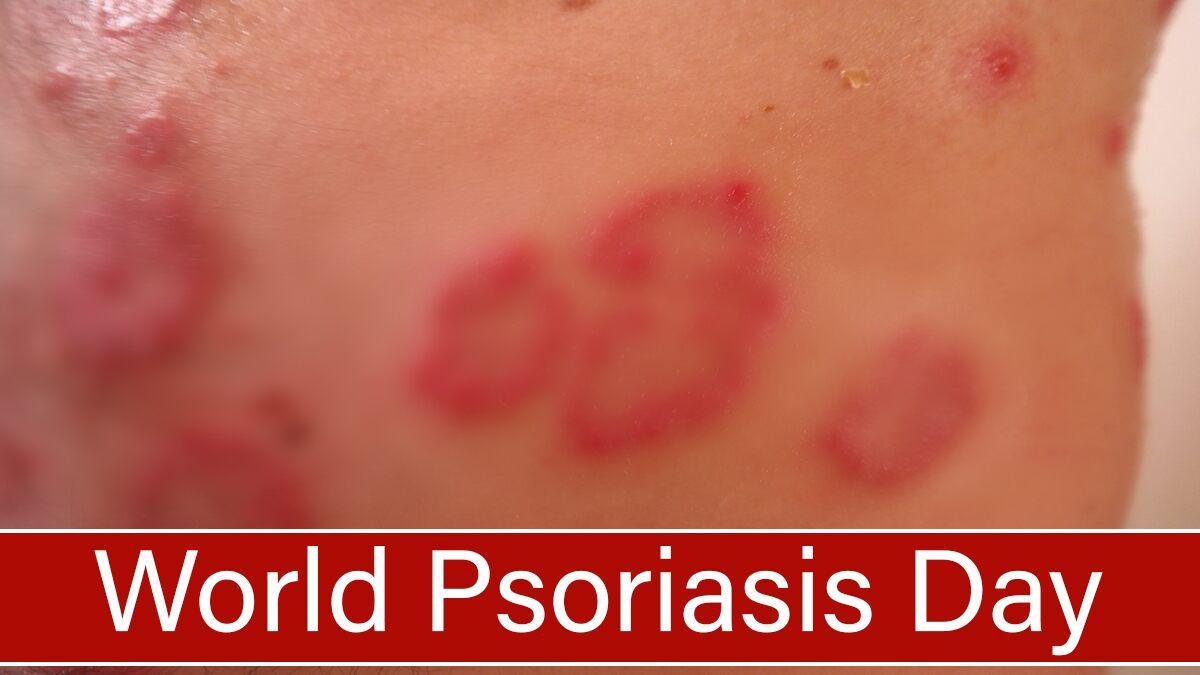
Because psoriasis primarily impacts the skin, many people assume it is merely a cosmetic problem. In reality, psoriasis is an autoimmune disease. This means that an overactive immune system is driving inflammation and overproduction of skin cells.
As with other autoimmune conditions, psoriasis patients may have a higher than average risk of contracting COVID-19 or developing serious complications, though more research on this patient population is needed. It is too preliminary to say whether or to what degree people with psoriasis could be affected differently by COVID-19.
An observational study that aims to determine how prevalent COVID-19 is in psoriasis patients who are using immunosuppressive medication is currently underway in Italy.
Recently, a study from the Perelman School of Medicine at the University of Pennsylvania found that psoriasis patients who use an IL-17 inhibitor were more likely to develop respiratory tract infections during previously conducted drug trials. They did not specifically look at risk for COVID-19, as these trials were conducted prior to the pandemic.
The flip side: IL-17 inhibitors have shown some promise as a potential treatment for COVID-19 patients who experience a cytokine storm.
Heres what you can do to stay healthy.
Common Autoimmune Disease Symptoms
Despite the varying types of autoimmune disease, many of them share similar symptoms. Common symptoms of autoimmune disease include:
- Fatigue
- Abdominal pain or digestive issues
- Recurring fever
- Swollen glands
Many women say its hard to get diagnosed, something that Orbai agrees with. Its not black or white, she says. Theres usually no single test to diagnose autoimmune disease. You have to have certain symptoms combined with specific blood markers and in some cases, even a tissue biopsy. Its not just one factor.
Diagnosis can also be difficult because these symptoms can come from other common conditions. Orbai says women should seek treatment when they notice new symptoms.
If youve been healthy and suddenly you feel fatigue or joint stiffness, dont downplay that, she says. Telling your doctor helps him or her to look closer at your symptoms and run tests to either identify or rule out autoimmune disease.
Autoimmune Disease: Why Is My Immune System Attacking Itself?
Autoimmune disease affects 23.5 million Americans, and nearly 80 percent of those are women. If you’re one of the millions of women affected by this group of diseases, which includes lupus, rheumatoid arthritis and thyroid disease, you may be wondering why your immune system is attacking itself.
Also Check: Does Selsun Blue Help With Psoriasis
What Happens During Psoriasis Autoimmune Attacks
In people with psoriasis, the immune system attacks autoantigens on tissues in the skin. These autoantigens include protein products made by the skin cells. Studies have identified the presence of these autoantigens in psoriatic lesions.
Autoantigens are believed to activate T cells and other cells of the immune system. T cells can destroy tissue and produce inflammatory chemicals such as interleukin-17A that promote the abnormal growth of skin cells.
Other immune cells, known as B cells, can also contribute to autoimmunity in psoriasis. B cells produce proteins known as antibodies that can help destroy antigens. In people with psoriasis and psoriatic arthritis , B cells make antibodies against the autoantigens associated with the skin. Antibodies made against autoantigens are referred to as autoantibodies.
Ultimately, the dysfunction and autoimmune activity of the immune system in psoriasis leads to the severe inflammation that contributes to overactive skin cell growth and psoriatic lesions or joint damage. High levels of inflammation from the overactive immune system may also be behind a higher risk for heart disease in people with psoriasis.
What Is An Autoimmune Disease
In an autoimmune disease, the body loses the ability to tell the difference between some of the bodys tissues and harmful microbes that can cause sickness, leading the body to attack healthy tissue.
The immune system is made up of cells and proteins that attack anything foreign to the body, such as invading bacteria, viruses, and other potential causes of infection and sickness. The immune system is designed to attack and neutralize invaders by recognizing molecules on them known as antigens. It is important that the immune system knows the difference between the bodys own tissues and a foreign invader.
However, when immune cells begin responding abnormally, they misidentify aspects of our own body as harmful invaders and attack. This abnormal response is described as being autoreactive or autoimmune auto is a Greek prefix meaning self. The self-antigens targeted in autoimmune diseases are known as autoantigens.
Autoimmune diseases are classified by the type of tissue that is being attacked. For example, in rheumatoid arthritis, the tissue lining the inside of the joints is attacked. In type 1 diabetes, the immune system attacks and destroys insulin-producing cells in the pancreas. In celiac disease, the immune system attacks the small intestine when gluten is consumed. And in people with psoriasis, the immune system produces inflammatory reactions against molecules related to the skin.
Don’t Miss: What Causes Scalp Psoriasis To Flare Up
Why Does The Immune System Attack The Body
Doctors dont know exactly what causes the immune-system misfire. Yet some people are more likely to get an autoimmune disease than others.
According to a 2014 study, women get autoimmune diseases at a rate of about 2 to 1 compared to men 6.4 percent of women vs. 2.7 percent of men. Often the disease starts during a womans childbearing years .
Some autoimmune diseases are more common in certain ethnic groups. For example, lupus affects more African-American and Hispanic people than Caucasians.
Certain autoimmune diseases, like multiple sclerosis and lupus, run in families. Not every family member will necessarily have the same disease, but they inherit a susceptibility to an autoimmune condition.
Because the incidence of autoimmune diseases is rising, researchers suspect environmental factors like infections and exposure to chemicals or solvents might also be involved.
A Western diet is another suspected risk factor for developing an autoimmune disease. Eating high-fat, high-sugar, and highly processed foods is thought to be linked to inflammation, which might set off an immune response. However, this hasnt been proven.
A 2015 study focused on another theory called the hygiene hypothesis. Because of vaccines and antiseptics, children today arent exposed to as many germs as they were in the past. The lack of exposure could make their immune system prone to overreact to harmless substances.
Things To Know About Psoriatic Arthritis
Learn more about what it means to have psoriatic arthritis.
1. PsA Is an Autoimmune Disease
2. It Has Ups and Downs, Called Flares
3. It Can Be a Master of Disguise
4. It Has Distinguishing Features
5. It Affects Up to a Third of People with Psoriasis
6. Its Gender Neutral
7. It May be Hereditary
8. Its Not Contagious
9. It Isnt Just About Your Joints
10. You May Not Look Sick
11. Effective Treatment is Available
Quick Links
Recommended Reading: What Vitamins Can Help Psoriasis
Setting The Stage: Psoriasis As An Immune
Figure 1. Complex fine-tuning of innate and adaptive immune mechanisms determines onset, course, and activity of psoriasis. As detailed in the text, intricate interactions between components of the innate with components of the adaptive immune system lie at the core of the pathophysiology of psoriasis. Once established, the relative contribution and fine-tuning of various mediators of adaptive and innate immunity determine the clinical manifestation toward chronic stable vs. highly inflammatory and/or pustular psoriasis.
What Is Psoriatic Arthritis
Psoriatic arthritis is an autoimmune disease the bodys own immune system becomes overactive and attacks normal tissues in the body. Patients with PsA can experience swelling, stiffness and pain in their joints and surrounding tissues, as well as nail changes and extreme fatigue.
According to the National Psoriasis Foundation , up to 30 percent of people with psoriasis will develop psoriatic arthritis. That means that PsA, which is an inflammatory form of arthritis, affects an estimated 2.25 million Americans.*
People with psoriatic arthritis experience the red patches of skin and silvery scales that psoriasis patients experience as well as the joint pain and stiffness associated with autoimmune forms of arthritis.
PsA can affect any part of your body, including your fingertips and spine, and the disease severity may range from relatively mild to severe. For patients with psoriatic arthritis, disease flare ups are relatively unpredictable as they often alternate with periods of remission.
There is currently no cure for psoriatic arthritis.
You May Like: Seborrheic Dermatitis Psoriasis On Face
How Psoriasis Is Diagnosed
A GP can often diagnose psoriasis based on the appearance of your skin.
In rare cases, a small sample of skin called a biopsy will be sent to the laboratory for examination under a microscope.
This determines the exact type of psoriasis and rules out other skin disorders, such as seborrhoeic dermatitis, lichen planus, lichen simplex and pityriasis rosea.
You may be referred to a specialist in diagnosing and treating skin conditions if your doctor is uncertain about your diagnosis, or if your condition is severe.
If your doctor suspects you have psoriatic arthritis, which is sometimes a complication of psoriasis, you may be referred to a doctor who specialises in arthritis .
You may have blood tests to rule out other conditions, such as rheumatoid arthritis, and X-rays of the affected joints may be taken.
When Should I Go To The Emergency Department
Go to the emergency department if any of the following autoimmune disease symptoms get severe:
- Trouble breathing/shortness of breath. Remember that some people with an autoimmune disease can experience this when theyre pregnant.
- Severe chest pain/pressure to your chest.
- A headache that starts suddenly and feels like the worst headache youve ever had.
- Sudden weakness, especially if you cant move.
- Dizziness that doesnt stop.
- Pain so severe that you cant stand it.
A note from Cleveland Clinic
Living with an autoimmune disease can be complicated. Diseases like lupus, rheumatoid arthritis and multiple sclerosis are complex and serious. Although there are no cures for these diseases, many of their symptoms can be treated, and sometimes they go into remission. Stay in touch with your healthcare provider about any advances in understanding and treating autoimmune diseases.
If you think you may have an autoimmune disease, see your healthcare provider as soon as possible for diagnosis and treatment. Your symptoms will be easier to control if the condition is treated promptly.
Last reviewed by a Cleveland Clinic medical professional on 07/21/2021.
References
Read Also: How To Stop Scalp Psoriasis
The Other Side: Antigen Presentation By Hla Molecules In Psoriasis
While most, if not all, autoimmune diseases are linked with certain HLA alleles , HLA-C*06:02 is the predominant psoriasis risk gene . HLA class I molecules present short peptide antigens to TCRs of CD8+ T cells. Such antigenic peptides are usually derived within the antigen presenting cell from parent proteins by proteasomal cleavage and loaded onto HLA-class I molecules. The HLA/peptide complex is then transported to the cell membrane where it can be recognized by CD8+ T cells . Thus, HLA-class I-restricted immune responses are usually directed against target cells which produce the antigenic peptide.
HLA-C*06:02-presented non-apeptides possess anchor amino acids at residues 2 and 9 , along with a putative anchor at residue 7 . HLA-C*06:02 features very negatively charged pockets and thus binds to distinct positively charged peptides. Given that between 1,000 and 3,000 different self-peptides have been detected on HLA-C*06:02 under experimental conditions, multiple cellular proteins should be, in principle, presented by this HLA molecule and recognizable by CD8+ T cells .
Help Make A Difference By Getting Involved Today

Signs and Symptoms of Psoriatic Arthritis
Onset of psoriatic arthritis is different for every patient. In some people it develops slowly with minimal symptoms but, in others it develops quickly and painfully. Early detection, diagnosis and treatment of psoriatic arthritis is critical to help prevent and/or limit the joint damage that can occur.
Here are common symptoms of psoriatic arthritis:
- General, overall fatigue
- Pain, swelling and/or tenderness around your tendons
- Reduced range of motion
- Stiffness and tiredness in the morning
- Swollen toes and finger
- Stiffness, pain, swelling and/or tenderness in your joint
- Nail changes
- Psoriatic arthritis usually affects the distal joints in fingers or toes
Your lower back, wrists, knees or ankle could also show signs and symptoms. In 85 percent of patients, psoriasis occurs before joint disease. If you have been diagnosed with psoriasis, it is important to tell your dermatologist if you have any aches and pains.*
Risk Factors For Psoriatic Arthritis
- Having psoriasis is the number one risk factor for developing psoriatic arthritis
- People with psoriasis on their nails have been shown to be even more likely to develop psoriatic arthritis
- Your family history is a risk factor as genetic component has been shown to exists with psoriasis and psoriatic arthritis patients.
- Anyone can develop psoriatic arthritis, but it occurs most often in adults between the ages of 30 and 50.
Also Check: Blue Star Ointment Good For Psoriasis
Screen For And Treat Comorbidities
If you have psoriasis, your dermatologist or primary care physician should screen you regularly â at least once a year â for PsA, says Dr. Ogdie.
âThe earlier you catch it and start treatment, the more likely you are to respond to therapy,â she says, noting that early treatment also potentially lowers the chances of permanent joint damage.
Dr. Ogdie advises people with psoriasis to understand the signs and symptoms of PsA. These include joint pain, swelling and tenderness â particularly in fingers and toes â and enthesitis, or inflammation at the points where tendons insert into bones. In addition, having psoriasis in the nails, scalp or skinfolds should raise suspicion for PsA, as should a family history of the disease.
âIf you have new symptoms, tell your doctor,â Dr. Ogdie says. âRemind them you have psoriasis and ask if these changes could mean you have psoriatic arthritis.â
Comorbidities such as CVD and metabolic syndrome can start developing at young ages in people with psoriasis and PsA, and sometimes health care providers arenât looking for them, Dr. Mehta says.
âPeople with psoriasis should ask their doctors to screen them for heart and metabolic disease. They can do this by checking the three âBs,â which are blood pressure, body mass index and blood levels of glucose and cholesterol,â he says.
Psoriasis = An Autoimmune Disease
Its taken years, but most researchers now classify psoriasis as an autoimmune disease. At the very least, they recognize a link between the two.
Its not hard to understand why. Folks with psoriasis have overactive T cells your immune systems personal fighter jets just like folks with other autoimmune diseases.
During a psoriasis flare-up, your T cells attack healthy skin cells with a special protein called cytokines. The cytokines make your skin cells multiply super fast so much so that they start building up on top of each other. This forms those dry, scaly patches.
In 2017, researchers confirmed that cytokines are involved in triggering psoriasis, which was a major milestone in the development of treatments.
Since then, research continues to indicate that immunosuppressants help with psoriasis.
Recommended Reading: What Is Guttate Psoriasis Pictures
What Are The Different Types Of Psoriasis
There are several significant classes of psoriasis:
Plaque psoriasis: It is the most common type of psoriasis. It occurs when new skin cells form too quickly, piling up on top of one another in thick, scaly patches that are red and itchy. This type of psoriasis accounts for about 80 percent of all cases.
Guttate psoriasis: This type of psoriasis occurs in children and young adults. Small, red, or purple-colored spots appear on the trunk and sometimes on the limbs. The sites are often itchy and may occur after a streptococcal throat infection. This condition tends to go away on its own after a few months.
Inverse psoriasis: In this form of psoriasis, the skin is smooth instead of scaly. Inverse psoriasis usually appears inside skin folds that rub together, such as under the breasts, between fingers and toes, armpits, or groin. This form also tends to go away without treatment within a year or two.
Pustular psoriasis: In this type of psoriasis, abnormal skin cell growth is accompanied by pus-filled blisters and redness. Pustular psoriasis can occur alone or in combination with other types of psoriasis. It tends to be more severe than other forms and may require hospitalization for treatment.
Erythrodermic psoriasis: It appears when plaque psoriasis or guttate psoriasis spreads over your entire body, causing widespread redness and peeling of your skin. This type of psoriasis can be severe and requires immediate medical attention.
How Is Psoriasis Genetically Inherited
Psoriasis has a strong genetic link when one parent carries two defective genes for any of several main forms of psoriasis, there is approximately a 20% chance that their children will have the disease. There are also several less common gene patterns associated with an increased risk of developing psoriasis. Researchers are currently working to understand better these patterns and why they contribute to autoimmune diseases like psoriasis.
Don’t Miss: Cuã¡l Es La Mejor Crema Para La Psoriasis