Psoriasis Is At Least Partially Genetic
Psoriasis tends to run in families, and a family history of the condition is considered a risk factor for the disease.
Researchers have found genes associated with the development of psoriasis in a region of the genome known as psoriasis susceptibility 1, or PSORS1. This gene accounts for up to 50% of the heritability referring to the genetic component of psoriasis and is usually associated with the condition developing earlier in life, typically before 40 years of age.
Genes in this region instruct the body to build proteins involved in the recognition of molecules called antigens, which trigger a persons immune responses. Typically, these antigens occur on the surface of foreign invaders, such as bacteria or viruses.
However, mutations in these genes can cause the immune system to incorrectly identify their own cells as foreign, leading to what is known as autoimmunity.
Studies have identified several other genes that also contribute to the development of psoriasis. These genes regulate many different processes, including:
- inflammation
Several factors associated with psoriasis may affect the immune system.
What Is An Autoimmune Disorder
Your body’s immune system is responsible for fighting foreign invaders threatening your health: bacteria, viruses, and fungi are just a few examples. Your good health depends partly on two important features of the immune system:
Unfortunately, when you have an autoimmune disease, your body’s immune system mistakenly confuses what is “self” with what is “other.” Instead of protecting your body, the immune system produces cells and chemicals that attack your own body, causing damage and disease.
There are many different autoimmune diseases, including psoriasis, rheumatoid arthritis, some types of thyroid diseases, some forms of anemia, lupus, celiac disease, and type 1 diabetes.
Psoriasis: A Genetic Analysis
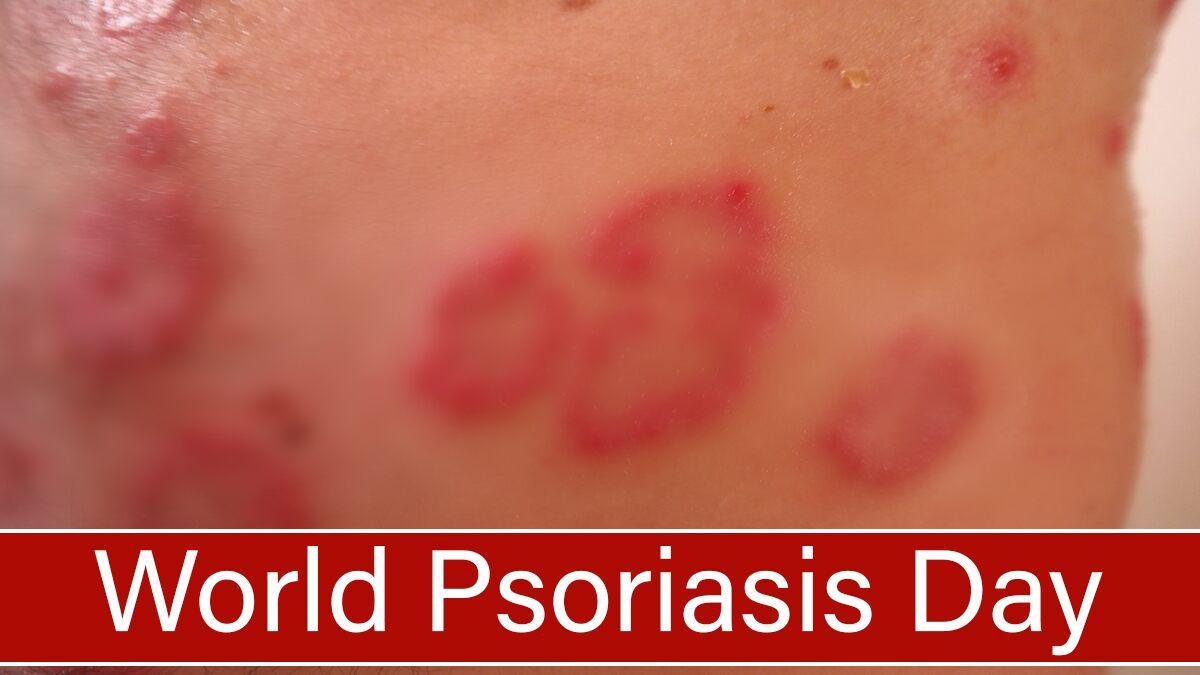
IntroductionPsoriasis is a fairly common autoimmune disease in which the body perceives the skin as foreign, and begins to attack it from within. This attack causes skin cells to reproduce rapidly causing red scaly patches of skin that will bleed when it becomes dry and cracked. This is a chronic illness that has no long term treatments, which means that managing flare-ups is extremely difficult. Since the majority of the world is unaware of psoriasis, people who suffer from the disease are often regarded
Don’t Miss: What Can I Put On Psoriasis
Thyroid Disease Research Paper
This disease is something that affects my everyday life and makes my normal routine very hard. My family at least my main family that is almost every single one of us has thyroid. We are a family of 13 6 girls and 4 boys counting my parents thats 13 right now I think only two of my siblings dont have it but are close to getting it. Often times, I find myself depressed and tired. More symptoms are pain in your joints, impaired memory, irregular periods cold, weakness and a puffy face there are
Treatments That Target The Immune System

Treatment for psoriasis depends on the type and severity of the condition, your general health, and other factors.
Here are the various treatments that target specific factors in the immune system that cause inflammation. These are generally used when your psoriasis symptoms are moderate to severe. Note that the newer drugs are more expensive.
Recommended Reading: Psoriasis On Face Around Nose
Alopecia Areata Can Cause Large Bald Spots
If you start losing large amounts of hair creating large bald spots, it may be due to alopecia areata, a condition where the immune system attacks the hair follicles in otherwise healthy people. This disease is marked by hair loss that occurs in round patches. You may lose all the hair on your scalp or body.
Alopecia areata is an unpredictable disease, and there is no cure. Hair growth sometimes restarts on its own, or there are treatments to spur regrowth. Your dermatologist can inject your scalp with corticosteroids and prescription creams may also help. Minoxidil, which is now available over the counter, is safe for children and adults to use. While you work with your doctor on treating alopecia, you may want to try changing your hairstyle to cover the alopecia patches or temporarily using a hair piece, suggests Dr. Simzar.
Why Psoriasis Is An Autoimmune Condition
Casey Gallagher, MD, is board-certified in dermatology. He is a clinical professor at the University of Colorado in Denver, and co-founder and practicing dermatologist at the Boulder Valley Center for Dermatology in Colorado.
Psoriasis causes a variety of symptoms that range from merely irritating to actually debilitating. The symptoms can include thick, red patches on the skin pitted, ridged fingernails scaly, itchy scalp and hair loss and stiff, painful joints.
Why do some people, but not others, get this frustrating condition in the first place? Arriving at an answer to this question relies partly on knowing that psoriasis is an autoimmune disorder “auto” meaning self and “immune” referring to the body’s complex immune system.
Don’t Miss: Does Psoriasis Affect Your Nails
Thyroid Disease Can Cause Dry Skin Hair Loss And Weight Gain
An underactive thyroid means you are producing too few thyroid hormones, in turn, your metabolism may slow down. Symptoms of hypothyroidism develop over time and may include dry skin, hair loss, weight gain, fatigue, and a sensation of being cold. Often hypothyroidism is a result of Hashimoto’s disease, when the immune system attacks the thyroid.
Hypothyroidism cant be cured, but it is generally easy to treat. You will have to take a synthetic form of the hormone as a daily pill. Periodic blood tests will help your doctor ensure you are taking the right dose. Once you have the condition under control, your symptoms will start to improve.
Systemic Autoimmune Rheumatic Diseases And Coinciding Psoriasis: Data From A Large Single
Anna Bazsó
1National Institute of Rheumatology and Physiotherapy, Frankel Leó Utca 38-40, Budapest 1023, Hungary
2Institute of Immunology, Rikshospitalet, Oslo University Hospital, 0027 Oslo, Norway
Abstract
Psoriasis is a systemic immune-inflammatory disease characterized by chronic or recurrent skin symptoms, psoriatic arthritis, enthesopathy, and uveitis. Psoriasis has recently been published to appear with various autoimmune disorders, but the coexistence has been systematically reviewed by only few studies until now. In the present study, charts and electronic database of 4344 patients with various systemic autoimmune disorders, under regular medical control at our department, were reviewed retrospectively searching for association with psoriasis. Hereby, we demonstrate 25 psoriatic patients coinciding with various systemic autoimmune diseases. The coexistence of psoriasis and autoimmune diseases resulted in the worsening of the clinical outcome of the autoimmune diseases as indicated by higher frequency and dosages of glucocorticoid use, need for biologicals, and other comorbidities. These results suggest common environmental and genetic background as well as therapeutic possibilities in the future.
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Summary
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Also Check: How To Treat Severe Psoriasis
Psoriasis: A Genetic Disease
Psoriasis is a genetic disease due to a misstep occurring in the way that a gene works. It is an autoimmune disease, meaning it has an abnormal response to a body part. Psoriasis is an inflammatory skin condition. Color change associated with the plaques is more obvious where there is little scaling of the skin . There are many different forms of psoriasis this disease can be found just about anywhere on the body. It is also associated with other health
Not Alone: Relations And Similarities Of Psoriasis With Other Autoimmune And Autoinflammatory Disorders
The highlights outlined so far show that both adaptive and innate immune processes contribute to psoriasis. Their balance and fine-tuning seem to determine the development of certain clinical forms of the disease, but also organ-specific manifestations. On the one hand, the outlined long-term systemic inflammatory processes probably contribute to the pathogenesis of important metabolic, cardiovascular, and mental concomitant diseases. In these areas, the evidence of a causal relationship is becoming increasingly clear and numerous publications prove this. A more detailed overview can be found elsewhere in this thematic focus. On the other hand, the contoured adaptive and innate immune mechanisms are not specific for psoriasis. Rather, many of them have been foundin varying degrees and weightingsin a whole range of other autoimmune and autoinflammatory diseases. In any case, although this interplay of different components of the immune system is certainly not yet fully understood, parallels with other chronic inflammatory and autoimmune diseases emerge that underpin our current view of psoriasis as a systemic disease.
Similar functional imbalances between Th17 and regulatory T cells as well as similar central cytokines including TNF, IL-23, and IL-17A, but also IL-1, IL-6, IL-17F, and IL-21 contribute to both diseases . Such striking parallels result in the response of both disorders to the same therapies.
You May Like: Hydrocortisone Cream For Psoriasis On Face
Psoriasis = An Autoimmune Disease
Its taken years, but most researchers now classify psoriasis as an autoimmune disease. At the very least, they recognize a link between the two.
Its not hard to understand why. Folks with psoriasis have overactive T cells your immune systems personal fighter jets just like folks with other autoimmune diseases.
During a psoriasis flare-up, your T cells attack healthy skin cells with a special protein called cytokines. The cytokines make your skin cells multiply super fast so much so that they start building up on top of each other. This forms those dry, scaly patches.
In 2017, researchers confirmed that cytokines are involved in triggering psoriasis, which was a major milestone in the development of treatments.
Since then, research continues to indicate that immunosuppressants help with psoriasis.
Why Is Psoriasis An Autoimmune Disorder
As part of its defense against foreign invaders, your body makes specialized white blood cells called T-cells. Under normal circumstances, T-cells identify and coordinate attacks on foreign invaders.
However, when you have psoriasis, your T-cells mistakenly identify your skin cells as invaders and attack them. This attack injures the skin cells, setting off a cascade of responses in your immune system and in your skin, resulting in the skin damage seen in psoriasis swelling, reddening, and scaling.
In an effort to heal, your skin cells begin reproducing much more rapidly than normal, and large numbers of new skin cells push their way to the surface of your skin. This occurs so quickly that older skin cells and white blood cells aren’t shed quickly enough. These discarded cells pile up on the surface of the skin, creating thick, red plaques with silvery scales on their surface: the hallmark of the classic form of plaque psoriasis.
Recommended Reading: How To Reduce Psoriasis Flare Ups
Narrative Essay On Autoimmune Disorder
permanent, I was finally diagnosed with a chronic autoimmune disorder, plaque psoriasis. Unfortunately, this sense of hopelessness my parents endured in those first months after my diagnosis was all too familiar. Although psoriasis was foreign to me, I became aware of what it meant to be chronically
Zagazig University Faculty Of Medicine Rheumatology
Zagazig UniversityFaculty of Medicine Rheumatology and Rehabilitation DepartmentSerum Interleukin-23 Level in Patients With Rheumatoid Arthritis and its Correlation with Disease Activity and Severity Protocol of thesisSubmitted for partial fulfillmentOf M.Sc. DegreeIn Rheumatology and RehabilitationByEnas Tawkal EldesokyMB.B.ChResident of Rheumatology and RehabilitationAt Dekrens General HospitalUnder supervision of Pro. Dr.
Read Also: Psoriasis On Bottom Of Foot
When To See A Doctor
Pityriasis rosea is not a severe condition, and it often resolves without leaving a trace. However, people with signs of pityriasis rosea should still visit a doctor to rule out other conditions. If they are experiencing severe itching, they can also ask for a prescription cream to provide relief.
People who have symptoms of psoriasis should visit a doctor for diagnosis and treatment. Anyone who also has any signs of infections, such as pain, swelling, or fever, should seek immediate medical care.
Psoriasis As A Spectrum Of Autoimmune To Autoinflammatory Processes
Psoriasis, as discussed above, exists on both a clinical and immunological spectrum in a delicate balance between adaptive and innate immune responses. On one end there is chronic plaque psoriasis where adaptive immune responses dominate, and on the opposite end there is generalized pustular psoriasis where the innate immune system and IL-36 autoinflammatory responses drive and dominate the inflammatory responses . Interestingly, while elevated in both plaque and pustular psoriasis, IL1B does not appear to have as critical role, and IL-1 antagonists are generally not effective in psoriasis, although some reports have suggested efficacy in generalized pustular psoriasis. Notably, clinical subtypes of psoriasis, such as erythrodermic and inverse psoriasis and localized pustular forms of psoriasis pustulosis palmoplantaris have IL-36 responses in-between those of plaque and pustular psoriasis . Therefore, psoriasis is a unique disease where each of its individual clinical phenotypes represents a different balance between autoimmune and autoinflammatory immune processes. Greater appreciation of these processes, and how they interact and feed into one another, will provide us with greater understanding of the disease processes involved in psoriasis and its clinical subtypes and provide new avenues for treatment.
Don’t Miss: Is Tumeric Good For Psoriasis
Dimethyl Fumarate Research Paper
Dimethyl fumarateDespite differences in symptoms, Multiple Sclerosis and Psoriasis are significantly linked, they are both immune-mediated and can be treated by the same drug: dimethyl fumarate. Multiple Sclerosis is an autoimmune disease in which the bodys immune system attacks the Myelin Sheath that covers a nerve cell in the CNS, thus causing scar tissue called Sclerosis.* Relapsing-Remitting Multiple Sclerosis involves episodes of inflammation called relapses which include: numbness
Common Pathogenesis Of Psoriasis And Aitd
Both abnormal immunological reactions and underlying genetic risk can contribute to the pathogenesis of psoriasis and AITD. These two diseases share some autoimmune processes and susceptibility genes, which may explain the concurrence of psoriasis and AITD. The predominant Th1 immune reaction has been observed in patients with psoriasis, such as Th1 infiltration in involved tissues, and high serum levels of Th1-prototype chemokines and cytokines , all of which are present in AITD. Additionally, Th17-mediated immune disorder has also been observed in psoriasis and AITD. The two diseases share several predisposing genetic alleles or regions. For example, the genetic data from 265 families with two or more autoimmune disorders have shown that the PTPN22-R620W allele has a remarkable association with HT and a mild association with psoriasis. Additionally, other SNP variations in the PTPN22 gene have been demonstrated to be indicators for evaluating the risk of psoriasis. IL12B has been generally recognised as a psoriasis susceptibility gene, an upstream variation of which affects the phenotype of AITD in men.
Recommended Reading: What Kind Of Doctor For Psoriasis
Psoriatic Disease Affects More Than Skin And Joints
The systemic inflammation that drives symptoms of psoriatic disease can raise your risk for other health problems.
If you have psoriasis or psoriatic arthritis , you may know that these diseases raise your risk for some other conditions as well. When one disease is triggered by or linked to another, the related condition is called a âcomorbidity.â PsA, for example, is a common comorbidity of psoriasis, affecting up to 33 percent of people with psoriasis.
According to the recent Joint AAD-NPF Guidelines of Care for the Management and Treatment of Psoriasis with Awareness and Attention to Comorbidities, other comorbidities for which psoriatic disease raises risk include:
- Cardiovascular disease
- Mental health impacts, including depression and anxiety
- Inflammatory bowel disease
- Uveitis
- Nonalcoholic fatty liver disease
Just how this elevated risk happens for each comorbidity isnât fully understood. One underlying factor that likely plays an important role in triggering or contributing to development of many comorbidities, however, is systemic inflammation, explains dermatologist Paul S. Yamauchi, M.D., Ph.D.
The weapons the immune system uses for this attack are inflammatory immune cells that normally defend the body from injury and infection.
The Link Between Psoriasis And Other Autoimmune Conditions

Psoriasis is a chronic disease that results in undesirable changes of the skin, including the development of thick, itchy, dry patches of skin. Psoriasis is thought to be caused by problems with the immune system. Specifically, overactive T cells mistakenly attack healthy skin cells and instigate other immune responses. Although your dermatologist can recommend effective psoriasis treatment options, its important to be aware that psoriasis can also increase your risk of additional autoimmune diseases.
Understanding Autoimmune Conditions
Autoimmune diseases can be particularly frustrating for patients because their immune systemswhich are supposed to keep patients healthyactually cause health problems. Normally, the function of the immune system is to detect and attack foreign invaders like viruses and bacteria. When a patient has an autoimmune disease, the immune system goes into attack mode despite the absence of pathogens. Instead, the immune system fights healthy body tissues like the skin and joints. The immune system accomplishes this by triggering an inflammatory response. In people with psoriasis, this inflammatory response manifests as skin plaques.
Identifying the Risks of Psoriasis
Facilitating Early Detection
Read Also: New Topical Treatments For Psoriasis
Psoriasis And Increased Risk For Autoimmune Thyroid Disease
The rate of autoimmune thyroid disease is significantly increased in patients with psoriasis, according to study data published in BMJ Open.
Researchers conducted a meta-analysis of the current evidence regarding the relationship between psoriasis and AITD after performing a literature search for relevant observational studies published before November 1, 2021. Eligible studies included at least 50 patients with psoriasis and control individuals.
A total of 11 studies with 253,313 patients with psoriasis and 1,376,533 control individuals were included in the final analysis. Among the included studies, 2 were cohort studies, 8 were case-controlled studies, and 1 was a cross-sectional study.
Patients with psoriasis had a higher prevalence of AITD compared with control individuals . The prediction interval was 0.79 to 2.73, with severe heterogeneity observed .
Patients with psoriasis had a higher prevalence of hypothyroidism compared with control individuals , with no significant heterogeneity . Patients with psoriasis also had an increased prevalence of hyperthyroidism vs control individuals , with no significant heterogeneity .
A significantly higher rate of thyroglobulin antibodies was observed in patients with psoriasis vs control individuals , with mild heterogeneity . The positive rate of thyroid peroxidase antibodies was significantly elevated in patients with psoriasis compared with control individuals , with moderate heterogeneity .
Reference