Psoriasis As A Spectrum Of Autoimmune To Autoinflammatory Processes
Psoriasis, as discussed above, exists on both a clinical and immunological spectrum in a delicate balance between adaptive and innate immune responses. On one end there is chronic plaque psoriasis where adaptive immune responses dominate, and on the opposite end there is generalized pustular psoriasis where the innate immune system and IL-36 autoinflammatory responses drive and dominate the inflammatory responses . Interestingly, while elevated in both plaque and pustular psoriasis, IL1B does not appear to have as critical role, and IL-1 antagonists are generally not effective in psoriasis, although some reports have suggested efficacy in generalized pustular psoriasis. Notably, clinical subtypes of psoriasis, such as erythrodermic and inverse psoriasis and localized pustular forms of psoriasis pustulosis palmoplantaris have IL-36 responses in-between those of plaque and pustular psoriasis . Therefore, psoriasis is a unique disease where each of its individual clinical phenotypes represents a different balance between autoimmune and autoinflammatory immune processes. Greater appreciation of these processes, and how they interact and feed into one another, will provide us with greater understanding of the disease processes involved in psoriasis and its clinical subtypes and provide new avenues for treatment.
The Link Between Psoriasis And Other Autoimmune Conditions
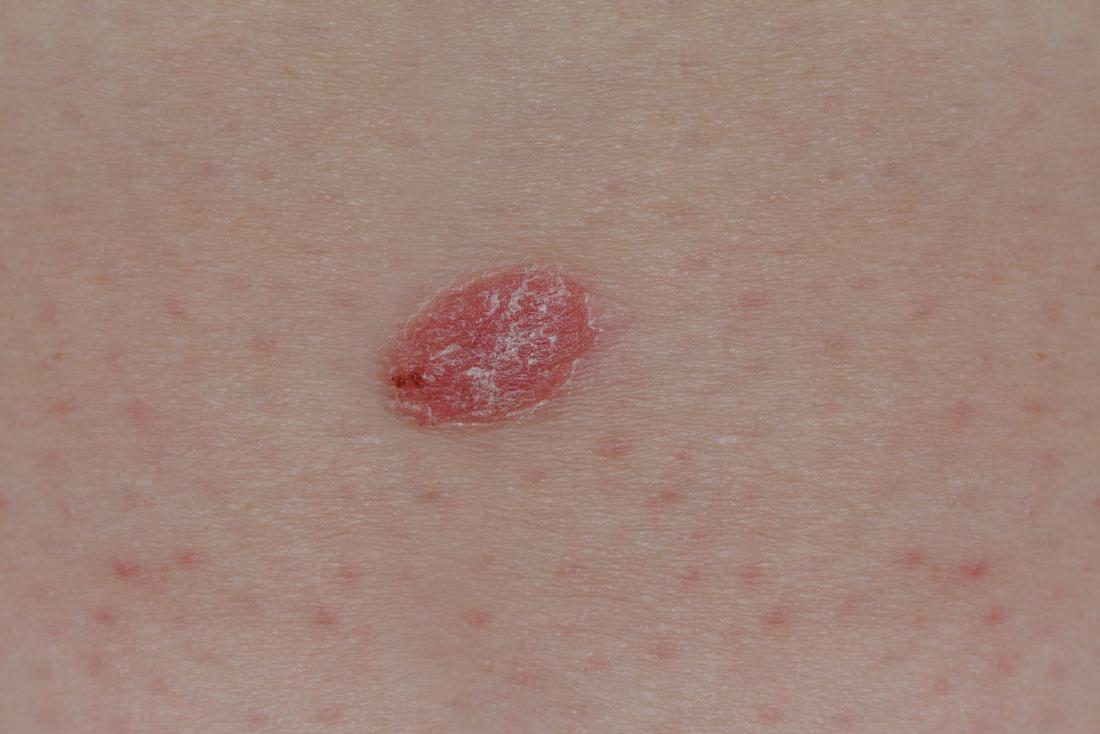
Psoriasis is a chronic disease that results in undesirable changes of the skin, including the development of thick, itchy, dry patches of skin. Psoriasis is thought to be caused by problems with the immune system. Specifically, overactive T cells mistakenly attack healthy skin cells and instigate other immune responses. Although your dermatologist can recommend effective psoriasis treatment options, its important to be aware that psoriasis can also increase your risk of additional autoimmune diseases.
Understanding Autoimmune Conditions
Autoimmune diseases can be particularly frustrating for patients because their immune systemswhich are supposed to keep patients healthyactually cause health problems. Normally, the function of the immune system is to detect and attack foreign invaders like viruses and bacteria. When a patient has an autoimmune disease, the immune system goes into attack mode despite the absence of pathogens. Instead, the immune system fights healthy body tissues like the skin and joints. The immune system accomplishes this by triggering an inflammatory response. In people with psoriasis, this inflammatory response manifests as skin plaques.
Identifying the Risks of Psoriasis
Facilitating Early Detection
How Do You Develop Psoriasis
The exact cause of psoriasis isnt fully understood. Its thought that overactive T cells, which are cells that fight off viruses and bacteria in your body, are involved. In people with psoriasis, T cells attack healthy skin cells and activate other immune responses. This increases the production of healthy skin cells, T cells, and other white blood cells.
As a result, too many skin cells accumulate on the skins outer layer. This is why some types of psoriasis cause the skin to have a scaly appearance. It normally takes weeks for new skin cells to form, but in people with psoriasis, skin cells form within days. The body doesnt shed the excess cells and psoriasis lesions occur.
People with a compromised immune system, including those with HIV or those who get repeated infections, have a higher risk of getting psoriasis.
Many environmental and lifestyle factors may trigger psoriasis flares. Not everyone with psoriasis has the same triggers. Common triggers are:
- sun exposure
- skin trauma, such as cuts, bug bites, and burns
- stress
- certain medications, such as lithium, blood pressure medications, and iodides
- heavy alcohol use
Smoking isnt just a psoriasis trigger. It may also be involved in its development and increase the severity of the disease.
Research shows that smoking may cause one in five cases of psoriasis and doubles your risk of getting the condition. This may be due to the effects of nicotine on skin cells, skin inflammation, and your immune system.
Also Check: Is L Lysine Good For Psoriasis
The Impact Of Psoriatic Disease Comorbidities
Psoriasis and PsA, and the comorbidities they lead to, can shorten your life. âPeople with psoriasis tend to live a few years less than those without the condition. This is particularly true for those with severe disease,â says Dr. Yamauchi. âItâs not the psoriasis thatâs shortening life span, but the heart attacks, strokes and other comorbidities it can cause.â
Letâs look at how some common comorbidities of psoriatic disease can affect your life and health.
Psoriasis And The Immune System

disagree . One alternative theory is that psoriasis occurs because the immune system reacts irregularly to bacteria on the skin due to genetics.
In an autoimmune disease, specific triggers cause the immune system to malfunction. These triggers vary between individuals. But in the case of psoriasis, they can include stress and skin trauma, such as insect bites, sunburn, and scratches.
In psoriasis, the activated immune system mistakenly launches an inflammatory response. It begins to attack healthy cells as though they were harmful invading pathogens. White blood cells called T helper lymphocytes, or T cells, become irregularly active and produce excess signaling molecules.
These cytokine molecules cause the blood vessels in the skin to widen. In turn, this causes white blood cells to accumulate, and keratinocytes, which make up the outer layer of the skin, to multiply much faster than usual.
In psoriasis, the process of a cell dividing, maturing, migrating to the skins surface, and sloughing off is complete in as few as 37 days, compared with 34 weeks in a person without psoriasis.
The result of this skin buildup is thickened, flushed, and scaly skin plaques.
| extra-virgin olive oil |
Recommended Reading: Does Methotrexate Help With Psoriasis
Psoriasis: A Genetic Analysis
IntroductionPsoriasis is a fairly common autoimmune disease in which the body perceives the skin as foreign, and begins to attack it from within. This attack causes skin cells to reproduce rapidly causing red scaly patches of skin that will bleed when it becomes dry and cracked. This is a chronic illness that has no long term treatments, which means that managing flare-ups is extremely difficult. Since the majority of the world is unaware of psoriasis, people who suffer from the disease are often regarded
How Long Does A Psoriasis Flare
People with psoriasis often have flare-ups . Flare-ups, or flares, are often the result of specific triggers, such as cold and dry weather, infection, illness, stress, dry skin, skin injuries, and the use of some medicines.
A psoriasis flare can last from a few weeks to a few months. Flares are usually followed by periods in which symptoms subside or go into remission.
A psoriasis flare-up is marked by red, dry, and thick skin patches. These patches sometimes contain silvery-white scales that itch or burn. The skin might become cracked and bleed. Psoriasis plaques frequently appear on the scalp, low back, knees, skinfolds , and genitals.
Additional symptoms of a psoriasis flare include:
- Nail changes: Pitting, thickening, ridges, crumbling, discoloration, and nail bed separation
- Emotional effects: Including depression and anxiety
- Joint symptoms: Including stiff, swollen joints if you have psoriatic arthritis, which affects up to 30% of people with psoriasis
Recommended Reading: Does Stress Cause Psoriasis Flare Ups
How To Prevent Psoriasis From Returning
There is no one-size-fits-all solution to managing psoriasis. If you are lucky enough to experience remission, you can take steps to keep your skin healthy and clear. Try the following strategies:
Expose skin to sunlight: Some sun exposure can help keep mild psoriasis at bay. Researchers recommend multiple but short sunlight exposures for people with psoriasis who can tolerate sunlight.
Manage stress: Since stress is a psoriasis trigger, it is good to relax and manage stress to keep inflammation from developing.
Avoid scrubbing: Scrubbing skin can irritate it and trigger a psoriasis flare. Wash your skin gently, pat dry, and moisturize.
Keep your body healthy: Staying healthy can reduce systemic inflammation. Ways to keep your body healthy include eating a nutritious, well-balanced diet, not smoking, being active, and restricting alcohol intake.
Monocytes Macrophages And Myeloid
Monocytes
Monocytes are known precursors for DCs and macrophages and as such, they have been described to be important cellular contributors to psoriatic pathology. It has been suggested that psoriatic monocytes engulf low density lipoprotein leading to overproduction of inflammatory cytokines. Additionally, psoriatic monocytes have also been described to possess increased phagocytic capabilities due to an imbalance in the ratio of cAMP/cGMP found in lesional skin. More recently an increase in CD14+ CD16+ intermediate monocytes termed Mon2 has been described in a cohort of human psoriatic patients., Interestingly, Mon2 monocytes also have been shown to be linked to an increased risk of CVD and to be predictive of myocardial infarction and death.
Macrophages
Myeloid-derived suppressor cells
You May Like: A& d Ointment For Psoriasis
What Happens If You Stop Treating Psoriasis
If a person stops treating psoriasis, progression of the disease is possible, and the condition will worsen with time. Psoriasis inflammation can also progress, which increases your risk for complications that affect the rest of the body.
According to The American Journal of Managed Care , untreated moderate-to-severe psoriasis can develop into PsA. PsA can be painful and disabling, and AJMC reports people with psoriasis and PsA have a more significant disease burden .
Additional complications of untreated psoriasis the increased risk for:
- Cardiovascular disease: Including heart attack, stroke, heart valve problems, and heart failure
- Metabolic syndrome: A combination of different metabolic disorders, including insulin resistance, elevated blood sugar, high cholesterol, high blood pressure, and abdominal obesity
- Type 2 diabetes: Condition in which the body does not correctly regulate and use sugar as fuel
- Anxiety and depression
- Inflammatory bowel disease: Inflammation of the gastrointestinal tract, including ulcerative colitis and Crohn’s disease
- Kidney disease: Condition in which the kidneys cannot filter blood normally, resulting in fluid and waste staying in the body
- Some cancers: Including squamous cell carcinoma, lymphoma, and basal cell carcinoma
- Serious and life-threatening infections
Cellular Participants In Psoriasis
The skin is a dynamic organ that serves as a front line defense against insults, injuries, and microbial pathogens. Given its constant exposure to the environment, immune surveillance and immune tolerance are key roles of the skin. The skin consists of the epidermis, dermis, and adipose tissue or subcutis layers. The epidermis is mainly composed of keratinocytes and Langerhans cells .
Recommended Reading: Psoriasis Relief Cream Gold Bond
If Psoriasis Strikes Again
If psoriasis strikes again, the best course of action is to treat it right away. You have many options for treatment, and new medication options are becoming rapidly available. Try different things to figure out what best keeps symptoms at bay and to keep psoriasis skin plaques from worsening or returning.
What Are Other Types Of Psoriasis
Plaque psoriasis is the most common type. About 80% to 90% of people with psoriasis have plaque psoriasis.
Other, less common types of psoriasis include:
- Inverse psoriasis appears in skin folds. It may look like thin pink plaques without scale.
- Guttate psoriasis may appear after a sore throat caused by a streptococcal infection. It looks like small, red, drop-shaped scaly spots in children and young adults.
- Pustular psoriasis has small, pus-filled bumps on top of the red patches or plaques.
- Sebopsoriasis typically appears on the face and scalp as red bumps and plaques with greasy yellow scale. This type is a cross between psoriasis and seborrheic dermatitis.
Also Check: Cbd Oil For Psoriasis Reviews
Genetics Adaptive Immune System And Evidence For Autoimmunity In Psoriasis
Of all the psoriasis studies that have been performed, genetic studies published in the last two decades have arguably provided the most robust insights into the critical pathogenic mechanisms in psoriasis. These have demonstrated that psoriasis is a complex genetic disorder involving multiple risk variants involved in various biological processes such as inflammation , antigen presentation, epidermal biology, cell signaling, and transcriptional regulation . It is worth noting that the great majority of studies done on the genetics of psoriasis have focused on the chronic plaque psoriasis subtype. Interestingly, when the risk genes are viewed through the prism of participation in either adaptive vs. innate immune system the genetic variants predisposing to chronic plaque psoriasis consist of a mixture of genes involved in either one of those two inflammatory axes .
What Exactly Is An Autoimmune Disease
When you have an autoimmune disease, your body mistakes normal, healthy tissues for foreign invaders. Basically, it goes to war with itself, causing damage and inflammation.
Not so fun fact: There are 100+ autoimmune diseases. Some of them, like psoriasis, only affects one body part . Others are system-wide, leaving your body exhausted and achy almost 24/7.
Regardless of your autoimmune diagnosis, your body is doing its war-waging thing because of some mysterious perfect storm of genetics and environmental factors.
Read Also: Psoriasis Spots All Over Body
Main Cytokines And Cell Types In Plaque Psoriasis
Disturbances in the innate and adaptive cutaneous immune responses are responsible for the development and sustainment of psoriatic inflammation . An activation of the innate immune system driven by endogenous danger signals and cytokines characteristically coexists with an autoinflammatory perpetuation in some patients, and T cell-driven autoimmune reactions in others. Thus, psoriasis shows traits of an autoimmune disease on an inflammatory background , with both mechanisms overlapping and even potentiating one another.
The main clinical findings in psoriasis are evident at the outermost layer of the skin, which is made up of keratinocytes. However, the development of the psoriatic plaque is not restricted to inflammation in the epidermal layer, but rather is shaped by the interaction of keratinocytes with many different cell types spanning the dermal layer of the skin. The pathogenesis of psoriasis can be conceptualized into an initiation phase possibly triggered by trauma , infection, or drugs and a maintenance phase characterized by a chronic clinical progression .
The pathogenesis of psoriasis.
The activation of the adaptive immune response via the distinct T cell subsets drives the maintenance phase of psoriatic inflammation . Th17 cytokines, namely IL-17, IL-21, and IL-22 activate keratinocyte proliferation in the epidermis.
Screen For And Treat Comorbidities
If you have psoriasis, your dermatologist or primary care physician should screen you regularly â at least once a year â for PsA, says Dr. Ogdie.
âThe earlier you catch it and start treatment, the more likely you are to respond to therapy,â she says, noting that early treatment also potentially lowers the chances of permanent joint damage.
Dr. Ogdie advises people with psoriasis to understand the signs and symptoms of PsA. These include joint pain, swelling and tenderness â particularly in fingers and toes â and enthesitis, or inflammation at the points where tendons insert into bones. In addition, having psoriasis in the nails, scalp or skinfolds should raise suspicion for PsA, as should a family history of the disease.
âIf you have new symptoms, tell your doctor,â Dr. Ogdie says. âRemind them you have psoriasis and ask if these changes could mean you have psoriatic arthritis.â
Comorbidities such as CVD and metabolic syndrome can start developing at young ages in people with psoriasis and PsA, and sometimes health care providers arenât looking for them, Dr. Mehta says.
âPeople with psoriasis should ask their doctors to screen them for heart and metabolic disease. They can do this by checking the three âBs,â which are blood pressure, body mass index and blood levels of glucose and cholesterol,â he says.
Read Also: What Is The Best Topical Cream For Psoriasis
Problems With The Immune System
Your immune system is your body’s defence against disease and it helps fight infection. One of the main types of cell used by the immune system is called a T-cell.
T-cells normally travel through the body to detect and fight invading germs, such as bacteria. But in people with psoriasis, they start to attack healthy skin cells by mistake.
This causes the deepest layer of skin to produce new skin cells more quickly than usual, triggering the immune system to produce more T-cells.
It’s not known what exactly causes this problem with the immune system, although certain genes and environmental triggers may play a role.
Psoriasis = An Autoimmune Disease
Its taken years, but most researchers now classify psoriasis as an autoimmune disease. At the very least, they recognize a link between the two.
Its not hard to understand why. Folks with psoriasis have overactive T cells your immune systems personal fighter jets just like folks with other autoimmune diseases.
During a psoriasis flare-up, your T cells attack healthy skin cells with a special protein called cytokines. The cytokines make your skin cells multiply super fast so much so that they start building up on top of each other. This forms those dry, scaly patches.
In 2017, researchers confirmed that cytokines are involved in triggering psoriasis, which was a major milestone in the development of treatments.
Since then, research continues to indicate that immunosuppressants help with psoriasis.
You May Like: Is Manuka Honey Good For Psoriasis
Psoriatic Disease Affects More Than Skin And Joints
The systemic inflammation that drives symptoms of psoriatic disease can raise your risk for other health problems.
If you have psoriasis or psoriatic arthritis , you may know that these diseases raise your risk for some other conditions as well. When one disease is triggered by or linked to another, the related condition is called a âcomorbidity.â PsA, for example, is a common comorbidity of psoriasis, affecting up to 33 percent of people with psoriasis.
According to the recent Joint AAD-NPF Guidelines of Care for the Management and Treatment of Psoriasis with Awareness and Attention to Comorbidities, other comorbidities for which psoriatic disease raises risk include:
- Cardiovascular disease
- Mental health impacts, including depression and anxiety
- Inflammatory bowel disease
- Uveitis
- Nonalcoholic fatty liver disease
Just how this elevated risk happens for each comorbidity isnât fully understood. One underlying factor that likely plays an important role in triggering or contributing to development of many comorbidities, however, is systemic inflammation, explains dermatologist Paul S. Yamauchi, M.D., Ph.D.
The weapons the immune system uses for this attack are inflammatory immune cells that normally defend the body from injury and infection.