What Are The Symptoms Of Psoriasis
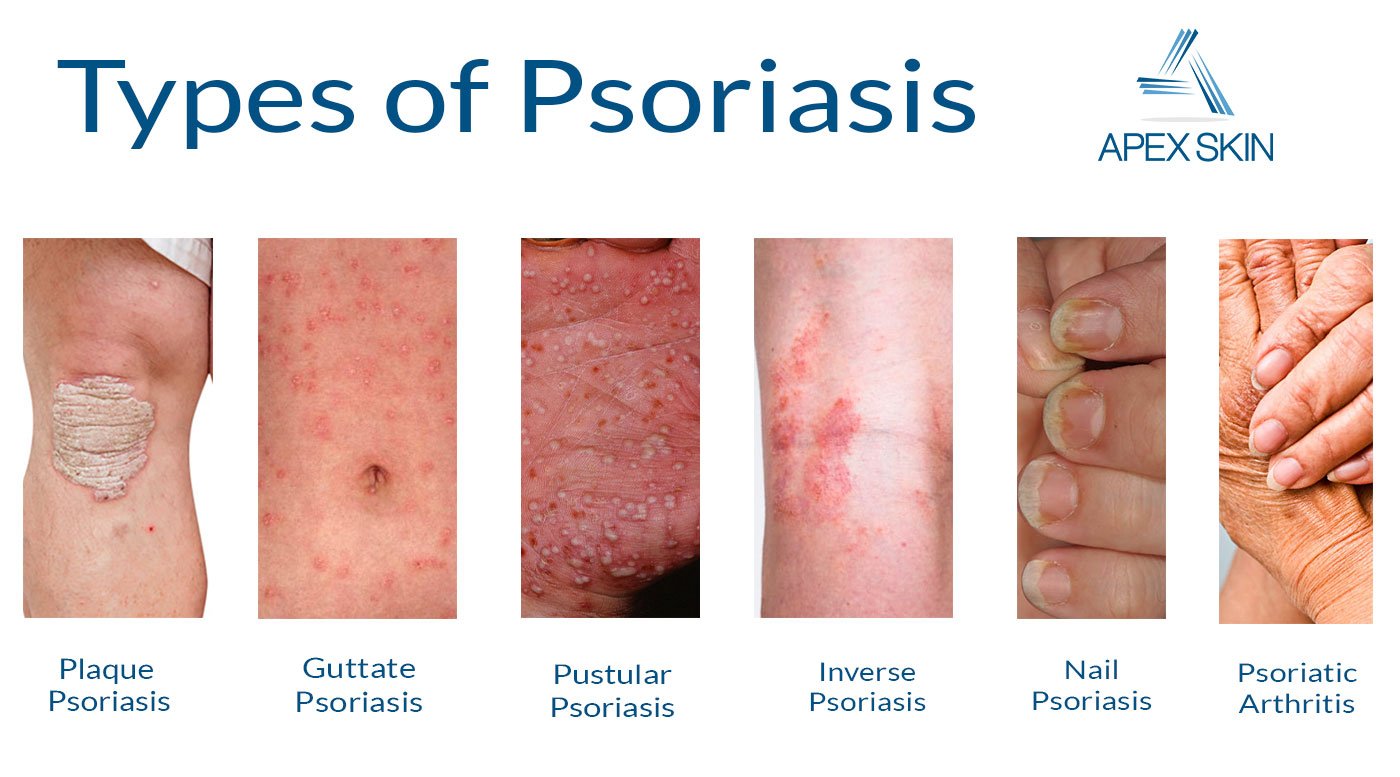
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Is There Vitamins N Inflammatory Arthritis
It is believed that nutritional supplements can help relieve joint pain, stiffness, and other symptoms related to arthritis. There are a number of natural products for diseases such as osteoarthritis and rhizitis that have been studied by researchers, among them glucosamine, silica gel, omega fatty acids, SAM-e, and curcumin.
Risk Factors For Psoriatic Arthritis
Youre at an increased risk for psoriatic arthritis if you have psoriasis. Family history of the condition also increases your risk. Many people with psoriatic arthritis have a parent or a sibling with the disease.
Age is another factor. People between the ages of 30 and 50 are at increased risk of developing psoriatic arthritis.
Also Check: How To Treat Genital Psoriasis Naturally
Diagnosing And Treating Psoriatic Arthritis
Having a physical exam is the first step to diagnosing and treating PsA. Your physician will talk with you about ongoing symptoms. Let your physician know if you have a family history of PsA, psoriasis or other autoimmune diseases. Your health care provider will also check for tenderness, swelling, limited movement, and skin or nail changes.
Read More: Aging With Arthritis
There is no cure for PsA. But that doesn’t mean you cant manage the disease and have a healthy, active life. You can work with your health care team to find the best treatment for you.
Treatment varies based on how the disease affects your life, Dr. Jones says. If you have mild symptoms, you may only need treatment during flare-ups. People with severe psoriatic arthritis may need a more aggressive treatment plan to reduce inflammation and improve quality of life.
When The Ntelligence D Gets Too Low

An insufficient amount of vitamin D can reduce bone strength, which also leads to osteoporosis and fractures. Also suffering from a Vitamin D deficiency can affect your health. Approximately 2% of children will experience digestive problems as a result of exposure. By accident, Rickets occurs when bones are swollen and fragile.
Also Check: Does Psoriasis Go Away And Come Back
Treating Psoriatic Arthritis And Skin Symptoms
- Psoriatic arthritis primarily causes joint pain and swelling, which can be reduced with treatments such as medication, physical therapy, or lifestyle changes.
- Most people with PsA also experience skin symptoms that can be relieved with other medications or light therapy.
- In order to treat the underlying factors that cause PsA, other medications called disease-modifying antirheumatic drugs are necessary.
Psoriatic arthritis, a form of arthritis that causes joint inflammation, most often leads to pain, stiffness, or swelling in the joints. Most people with PsA also have psoriasis, with symptoms such as patches of thickened, scaly skin or pitting of the nails.
In some cases, people diagnosed with PsA begin a treatment plan that involves separate treatments for joint symptoms and skin symptoms. This may work for some people, but it leaves others with ongoing symptoms. Those who follow this type of treatment plan may not realize that these therapies are not addressing the underlying sources of inflammation that are contributing to psoriatic arthritis and psoriasis.
When initial treatment stops working, people with PsA often switch to more aggressive treatment options. These target the underlying causes of disease, rather than only providing symptom relief. If your current therapies arent effectively managing your joint and skin symptoms, you may want to talk to your doctor about other possible treatment approaches.
Can Psoriatic Arthritis Affect Other Parts Of The Body
Having psoriatic arthritis can put you at risk of developing other conditions and complications around the body.
The chances of getting one of these are rare. But its worth knowing about them and talking to your doctor if you have any concerns.
Eyes
Seek urgent medical attention if one or both of your eyes are red and painful, particularly if you have a change in your vision. You could go to your GP, an eye hospital, or your local A& E department.
These symptoms could be caused by a condition called uveitis, which is also known as iritis. It involves inflammation at the front of the eye.
This can permanently damage your eyesight if left untreated.
Other symptoms are:
- blurred or cloudy vision
- sensitivity to light
- not being able to see things at the side of your field of vision known as a loss of peripheral vision
- small shapes moving across your field of vision.
These symptoms can come on suddenly, or gradually over a few days. It can affect one or both eyes. It can be treated effectively with steroids.
Heart
Psoriatic arthritis can put you at a slightly higher risk of having a heart condition. You can reduce your risk by:
- not smoking
- staying at a healthy weight
- exercising regularly
- eating a healthy diet, thats low in fat, sugar and salt
- not drinking too much alcohol.
These positive lifestyle choices can help to improve your arthritis and skin symptoms.
Talk to your doctor if you have any concerns about your heart health.
Crohns disease
Non-alcoholic fatty liver disease
Don’t Miss: Is Head And Shoulders Good For Psoriasis
It’s My Confirmed Diagnosis And I Stand By It
After living without a diagnosis for so long, I’m a little defensive of my diagnosis. So I’ve taken care to see rheumatologists and dermatologists who are very experienced in treating psoriatic disease, and I highly recommend others do the same.
When I found out I had to find a new doctor, I was so scared I wouldn’t find one who was as experienced. But thankfully, with the help of the internet, I found a rheumatologist who specialized in psoriatic disease.
She looked at my files, listened to my health history carefully, and caught a few small pits in my nails I hadn’t even noticed. And she confirmed- yes, Elizabeth, you can have psoriatic arthritis without psoriasis.
Is It Possible To Have Psoriatic Arthritis Without Psoriasis
People with the autoimmune disease psoriatic arthritis usually also have the skin condition psoriasisbut not always.
Experts in the field of psoriatic arthritis have long faced a chicken-and-egg question: Can you have psoriatic arthritis without having psoriasis first? Some say yes. Some say no. Others say yes and no.
“There is a lot of debate going on,” says Ted Mikuls, MD, professor of internal medicine in the division of rheumatology at the University of Nebraska Medical Center in Omaha.
Like psoriatic arthritis, psoriasis is an autoimmune disease, meaning the immune system attacks a part of the body. With psoriasis, the immune system attacks the skin , while psoriatic arthritis attacks the joints . About 80-85%of people who develop psoriatic arthritis have psoriasis first, according to the National Psoriasis Foundation. For the remaining 15-20%, arthritis precedes the skin condition.
“It is much, much more common to have the psoriasis first,” says Marcy OKoon Moss, senior director for consumer health at the Arthritis Foundation in Atlanta.
But the question remains: If a patient first experiences joint symptoms of psoriatic arthritis, does that mean they don’t have psoriasisor just that their psoriasis hasnt been detected yet?
RELATED: The 5 Types of Psoriatic Arthritis You Need to Know About
Recommended Reading: Is Activated Charcoal Good For Psoriasis
Can A Person Have Psoriatic Arthritis Without Psoriasis
Answer: It is certainly possible that a person could have both rheumatoid arthritis and psoriatic arthritis. However, doctors, including rheumatologists, generally avoid making multiple diagnoses when a single diagnosis could suffice.
PsA is an autoimmune disease, which means the body’s immune system.
It will get harder to move joints and someone may become disabled.
Like psoriasis, psoriatic arthritis is a chronic disease related to the immune.
This is why it’s important to get the correct diagnosis when symptoms.
If you think you might have psoriatic arthritis, you can learn more by.
this website is prohibited without written permission of National Psoriasis Foundation.
Life With Psoriatic Arthritis: Finding Balance Psoriatic arthritis is an inflammatory type of arthritis related to psoriasis that can cause joint pain, stiffness, and.
People with the autoimmune disease psoriatic arthritis usually also.
question: Can you have psoriatic arthritis without having psoriasis first?
Psoriatic arthritis can develop slowly with mild symptoms, or it can develop.
people can develop psoriatic arthritis without having psoriasis.
A person can have rheumatoid arthritis and psoriatic arthritis, but that is rare.
But we know that for about 85% of patients with psoriasis, the onset of psoriatic arthritis occurs in about 10 years. He said that a limited number of answers have begun to emerge.
anything from.
Without treatment, psoriatic arthritis may be disabling.
May 11, 2017.
Psoriatic Arthritis Vs Rheumatoid Arthritis
Because psoriatic arthritis impacts the skin as well as the joints, its sometimes referred to as a double whammy, or like rheumatoid arthritis but with a nasty skin rash, according to the arthritis advocacy group Creaky Joints.
Both psoriatic and rheumatoid arthritis are autoimmune disorders that cause joint inflammation, pain, and stiffness, as well as chronic fatigue. But there are differences in how the diseases develop and affect the joints.
According to Kathleen Maksimowicz-Mckinnon, DO, a rheumatologist at Henry Ford Hospital in Detroit, there are some telltale signs that your arthritis pain is due to psoriatic arthritis, and not rheumatoid arthritis. These include:
RELATED: Signs and Symptoms of Psoriatic Arthritis
Recommended Reading: How To Deal With Psoriasis On Face
What Causes Psoriasis And Psoriatic Arthritis
While no one knows the exact cause of psoriasis or PsA, experts believe that a faulty immune system is partly to blame. Specifically, the immune system attacks healthy skin cells and joints, causing the inflammation, swelling, and pain characteristic of psoriatic disease.
Genetics plays a part, too: Often will have other family members with psoriatic disease, says Dr. Haberman. In fact, roughly 40 percent of people with PsA have at least one close family member with psoriasis or psoriatic arthritis. Research is still ongoing, however, and its not clear whether having a family history of psoriasis alone increases PsA risk.
Obesity is also a common risk factor for people with psoriasis and PsA. According to a 2019 study in the journal Medicine, roughly 40 percent of people with psoriasis are obese. While it is unknown why obesity is so strongly linked to psoriatic diseases, we do know that obesity is associated with the production of inflammatory chemicals in the body, says Dr. Haberman. It may be that this underlying inflammatory environment helps predispose the body to the development of psoriasis and PsA, she says.
Other risk factors for psoriasis include:
- Family history
- Viral and bacterial infections
- Stress
- Obesity
- Smoking
- Alcohol consumption
Read more here about psoriatic arthritis risk factors.
Will Drug Treatments For Psoriatic Arthritis Make My Psoriasis Worse
Some drug treatments may make psoriasis worse, but then again, some can also make it better too. Before you start any treatments offered, discuss this both with your dermatologist and rheumatologist. DONT FORGET to politely request that both consultants let each other know of your treatment regimes, this helps both of them evaluate your treatment and any side effects that you may be likely to experience. Some people find that when their psoriasis is bad their arthritis is also bad and as one improves, so does the other. This most often occurs when the skin and joint disease start simultaneously. Some of the arthritis treatments also help the skin and this is can help the doctors decide which is the best drug to use.
Also Check: Does Humira Work For Psoriasis
Who Will Be Responsible For My Healthcare
Youre likely to see a team of healthcare professionals.
Your doctor, usually a rheumatologist, will be responsible for your overall care. And a specialist nurse may help monitor your condition and treatments. A skin specialist called a dermatologist may be responsible for the treatment of your psoriasis.
You may also see:
- a physiotherapist, who can advise on exercises to help maintain your mobility
- an occupational therapist, who can help you protect your joints, for example, by using splints for the wrist or knee braces. You may be advised to change the way you do some tasks to reduce the strain on your joints.
- a podiatrist, who can assess your footcare needs and offer advice on special insoles and good supportive footwear.
Treatment For Psoriatic Arthritis Differs From Other Forms Of Arthritis
The main goals of all arthritis treatment are to reduce symptoms and improve quality of life. Methods vary depending on the type of arthritis.
Rheumatoid arthritis can be very destructive if its not treated, which is why we treat it aggressively with biologics, says Ruderman. But psoriatic arthritis doesnt manifest that way. Fewer than half of people with psoriatic arthritis develop a particularly aggressive form, which makes treatment challenging because we dont want to over-treat it.
Even so, the pain and discomfort associated with psoriatic arthritis can be significant. A study published in 2015 in the journal PLoS One found that the overall pain, joint pain, and fatigue reported by psoriatic arthritis patients was significantly greater than that reported by people with rheumatoid arthritis.
Unless someone has an existing condition, such as elevated blood pressure or kidney disease, nonsteroidal anti-inflammatory drugs are recommended for joint symptoms in milder forms of psoriatic arthritis, says Husni.
Topical creams, ointments, and lotions are often used to address the scaly, itchy skin rashes that occur with psoriasis.
If there are signs of joint damage, doctors treat psoriatic arthritis more aggressively with medications like the ones used to treat rheumatoid arthritis, says Ruderman. These include disease-modifying anti-rheumatic drugs and biologics.
Additional reporting by Becky Upham.
Don’t Miss: Can Psoriasis Cause Weight Gain
How Will I Know If I Have Psoriatic Arthritis
In order for you to be diagnosed with psoriatic arthritis, you will be observed by the Arthritis Group. There is no dialogistic test for PsA, so you will work closely together to address your concerns and your medical history.
You may have to rule out other conditions including:
- Rheumatoid arthritis
How Should Patients With Psoriatic Arthritis Be Managed
The articular and dermatologic manifestations associated with PsA are remarkably heterogeneous in both the extent and type of tissue involvement. Patients with PsA, a chronic systemic inflammatory disorder, may develop not only peripheral arthritis but also axial disease, dactylitis, enthesitis, and skin and nail psoriasis, with consequent adverse impact on function and quality of life .
Heterogeneity is observed not only in disease manifestations but also in severity and course, which can vary from very mild psoriasis or enthesitis to widespread psoriatic plaques, disfiguring nail disease, and severe joint inflammation with destruction that can result in disability and increased mortality. Moreover, comorbidities associated with psoriasis, such as the metabolic syndrome, can contribute to damage in multiple end-organs and often leads to markedly impaired QOL as well as early mortality.
Management of patients with psoriatic arthritis
Another approach for patients who fail an anti-TNF is to add or switch a DMARD, although the combination of anti-TNF agents and DMARDs has not been formally evaluated in this disease. For patients who cannot take or are non-responders to anti-TNF agents, apremilast, ustekinumab, or secukinumab are effective alternatives approved for treatment of PsA.
Also Check: How To Control Scalp Psoriasis Naturally
Four Main Types Of Psoriatic Arthritis
There are 78 major joints in the body and psoriatic arthritis can affect any one of these. Usually, however, certain joints are more likely to be affected . Different patterns are found. Sometimes just one or two joints are a problem but often several joints, both large and small and on both sides of the body, are involved. About a third of people with psoriatic arthritis also have spondylitis which can result in a painful, stiff back or neck. Psoriasis can affect the nails with pitting, discolouration and thickening and this may be associated with inflammation in the joints at the end of the finger or toe. Another way in which psoriatic arthritis can be recognized is the finding of a sausage-like swelling of a finger or toe, called dactylitis. This is caused by inflammation occurring simultaneously in joints and tendons, painful heels and other bony prominence can also occur and this is caused by inflammation where gristle attaches to bone.
About Psoriatic Arthritis And Psoriasis
Psoriasis is a chronic, inflammatory disease that typically affects the skin. In about 80 percent of cases, psoriasis manifests as a scaly, itchy rash of skin plaques that most frequently affects the elbows, knees, and scalp.
PsA is characterized by inflammation of the tendons and ligaments. Symptoms of psoriatic arthritis include lower back pain, inflammatory joint pain, and joint swelling and stiffness. Often, psoriatic arthritis also affects the nails, causing nail changes and symptoms such as pitting small dents in your nails. Left untreated, PsA can cause lasting joint damage. Approximately 1 in 5 people with PsA will experience spinal inflammation, known as psoriatic spondylitis. In some instances, spinal inflammation is so severe, it can cause complete fusion of the vertebrae, known as ankylosing spondylitis.
You May Like: Psoriasis On Back Of Hands
Can Psoriatic Arthritis Affect Children Too
As many as 12,000 children in the UK are affected by arthritis. It is known as juvenile chronic arthritis , of which there are three main types, stills disease, polyarticular juvenile chronic arthritis and polyarticular onset juvenile chronic arthritis. Psoriatic arthritis is a minor subset of JCA and is uncommon.