Students Who Viewed This Also Studied
MN 553 Unit 1 Quiz with answers – Kaplan University TB1-18.pdf
University of Maryland, College Park
NURS 580
CH46 Upper Respiratory Infections, Otitis Media, and Otitis Externa.rtf
Nursing College
University of Maryland, College Park NURS 580
MN 553 Unit 1 Quiz with answers – Kaplan University TB1-18.pdf
test_prep
Chamberlain College of Nursing ADVANCED P NR508
WK 7 quiz.rtf
Nursing College MED SURG 211
CH46 Upper Respiratory Infections, Otitis Media, and Otitis Externa.rtf
Miami Dade College, Miami NUR chm1045
Chapter 33- Anticholinergic Agents
What Injections Or Infusions Are Available For Psoriasis
Recently, a new group of drugs called biologics have become available to treat psoriasis and psoriatic arthritis. They are produced by living cells cultures in an industrial setting. They are all proteins and therefore must be administered through the skin because they would otherwise be degraded during digestion. All biologics work by suppressing certain specific portions of the immune inflammatory response that are overactive in psoriasis. A convenient method of categorizing these drugs is on the basis of their site of action:
Drug choice can be complicated, and your physician will help in selecting the best option. In some patients, it may be possible to predict drug efficacy on the basis of a prospective patient’s genetics. It appears that the presence of the HLA-Cw6 gene is correlated with a beneficial response to ustekinumab.
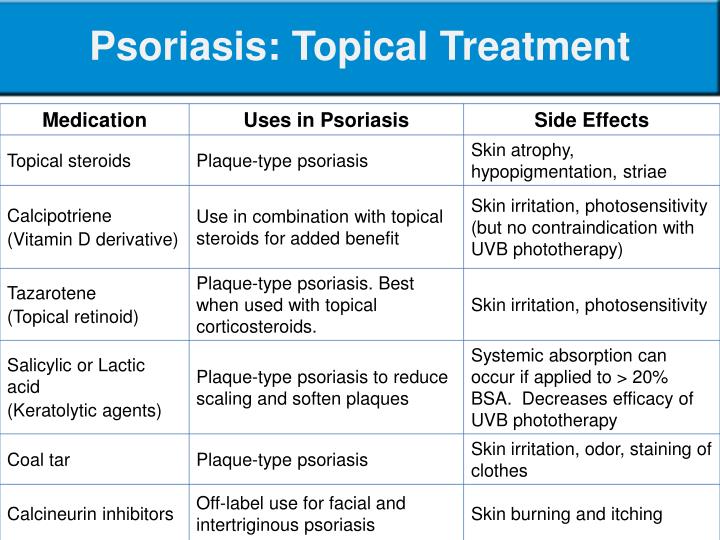
Vitamin D Analogues: How They Help
Vitamin D analogues are used to help control overactive skin cell production by binding to the vitamin D receptors on the skin cells.
Topical vitamin D analogues such as:
- calcitriol
are effective at slowing the growth of the skin cells and can be used with emollients and topical corticosteroids applied to the skin.
Calcipotriene with betamethasone is a vitamin D analogue that is already combined with an antiinflammatory corticosteroid. Brands include: Taclonex, Taclonex Scalp, Wynzora and Enstilar.
The most common side effect with these agents is mild skin irritation. Some topical vitamin D analogues may take up to 6 to 8 weeks for their full effect.
Oral calcitriol can also be used for psoriasis.
Also Check: What Does Psoriasis Scalp Look Like
Reviewing Treatment With Topical Medications
If you are an adult, your healthcare professional should arrange a review appointment 4 weeks after you start a new topical treatment. Children should have a review appointment 2 weeks after starting a new topical treatment.
If there is little or no improvement at this review, your healthcare professional should discuss the next treatment option with you and check if there are any reasons why the treatment is not working.
If your psoriasis is responding to topical treatment your healthcare professional should discuss with you:
-
the importance of continuing treatment until your psoriasis improves or for the length of time recommended
-
that relapse occurs in most people after treatment is stopped
-
that after the initial treatment period topical treatments can be used as and when you need them to control your psoriasis.
You should be offered a supply of your topical treatment to keep at home to use yourself as needed.
If you are an adult and have been using potent or very potent corticosteroids, your healthcare professional should offer you annual once-yearly review to check for problems. Children and young people who have been using corticosteroids of any strength should also have their treatment reviewed once a year.
The Goal Of Treatment: Satisfaction With Treatment And Outcome
Defining treatment goals determines adherence, manages expectations, and avoids treatment failures. Goals are important to provide patients with short- and long-term perspectives for their disease. The ultimate goal of psoriasis treatment is the complete clearance of all skin symptoms however, realistically, it is not possible to achieve this in all patients and/or cannot be permanently maintained because psoriasis is a chronic and recurring disease. Whereas a PASI 75/90/100 improvement and the more recently established absolute PASI 2 or Physician Global Assessment 0/1 are commonly used outcome parameters in clinical trials, those severity parameters are not regularly assessed by all physicians in daily practice for cases of mild-to-moderate psoriasis.
We are in consensus that patient satisfaction should be considered the primary criterion when assessing the goals and success of treatment.
In daily practice, the assessment of patient satisfaction can be done by asking a question that requires a simple answer Yes or No as to whether a patient is satisfied with the treatment or treatment outcome. If a patient is not satisfied, and before deciding on the next step, i.e., to continue or change the treatment, it is recommended that the cause of discontent be explored further by examining the following aspects:
Recommended Reading: Is Argan Oil Good For Psoriasis
Clinical Manifestation Of Psoriasis
Psoriasis is a chronic, inflammatory, multi-system disorder characterized by abnormal epidermal differentiation and hyperproliferation thought to be related to abnormal immune system activity. According to data from various resources, about 2-3% of the general population suffers from psoriasis. Accepting and extrapolating these rates globally, approximately 140 to 210 million people live with psoriasis Although psoriasis is usually benign, it is a lifelong illness with remissions and exacerbations and is sometimes refractory to treatment. Nonetheless, the majority of the cases are mild or moderate psoriasis . A recent study observed 75.8% of patients to have a psoriasis area severity index of < 20 . Moreover, 17-55% of patients experience remissions of varying lengths. Plaque-type psoriasis is the most common form, affecting 80 90% of patients. Inverse, erythrodermic, pustular and guttate forms of psoriasis have also been described. Patients present with sharply demarcated, erythematous plaques covered by silvery white scales, most commonly on the extensor surfaces and the scalp. The natural history is variable but is often chronic and relapsing, and patients may experience extracutaneous manifestations commonly including nail involvement and psoriatic arthritis in up to 20% of patients .
What Are Other Types Of Psoriasis
Plaque psoriasis is the most common type. About 80% to 90% of people with psoriasis have plaque psoriasis.
Other, less common types of psoriasis include:
- Inverse psoriasis appears in skin folds. It may look like thin pink plaques without scale.
- Guttate psoriasis may appear after a sore throat caused by a streptococcal infection. It looks like small, red, drop-shaped scaly spots in children and young adults.
- Pustular psoriasis has small, pus-filled bumps on top of the red patches or plaques.
- Sebopsoriasis typically appears on the face and scalp as red bumps and plaques with greasy yellow scale. This type is a cross between psoriasis and seborrheic dermatitis.
You May Like: Red Light Therapy For Psoriasis
Topical Treatment For Trunk And Limb Psoriasis In Adults
If you have psoriasis of the trunk or limbs you should be offered a potent corticosteroid and a vitamin D preparation as initial treatment. Each treatment should be applied once a day and should be used for up to 4 weeks.
If this does not improve or control your psoriasis, you should be advised to stop using the potent corticosteroid and apply only the vitamin D preparation twice a day for up to 8 weeks.
If the vitamin D preparation does not improve or control your psoriasis after 8 to 12 weeks, you should be offered one of the following treatments:
-
a potent corticosteroid to apply twice a day for up to 4 weeks or
-
a coal tar preparation applied once or twice daily or
-
a combined product containing a potent corticosteroid and vitamin D applied once a day for up to 4 weeks.
If these treatment options don’t control your psoriasis, you may be referred to a specialist who may offer you other topical treatments, or other treatment options depending on how extensive your psoriasis is and the impact the psoriasis is having on your life.
For some forms of localised psoriasis where other treatments have not been successful, your healthcare professional may offer you ‘short-contact’ dithranol ointment or cream. To ensure it is applied correctly, you should be given educational support to help you apply it yourself or treatment should be given in a specialist setting.
Treatment Of Psoriasis With Topical Agents
Submitted: May 29th 2012Reviewed: September 24th 2012Published: April 17th 2013
DOI: 10.5772/53759
- Michael G. DeGroote School of Medicine, Waterloo Regional Campus, McMaster University, Canada
Anupam Mitra
Laura Morrissey Rogers
Hermenio Lima*
DOI: 10.5772/53759
Also Check: Best Over The Counter Scalp Psoriasis Treatment
Is Psoriasis The Same As Eczema
Psoriasis and eczema are two different skin conditions. They differ in where the disease appears on the body, how much it itches and how it looks. Eczema tends to appear more often behind the knees and inside the elbows. Eczema also causes more intense itching than psoriasis. Many people, especially children, can get both eczema and psoriasis.
Immunomodulators Basic Concept Of Drugs Used To Treat Psoriasis
In a homeostatic situation, the immune system interacts with many antigens without notice in a healthy individual . However, the development of a hypersensitivity response induced by the chronic stimulation of the immune system results in the clinical manifestation of a specific group of illnesses . The lack of control of the immune response is the basis of the clinical manifestation of these diseases. In the majority of these cases, there is an increase in the immune response activity. Therefore, the manifestation of a hypersensitivity reaction induces the pathogenesis of autoimmune and other inflammatory diseases .
The basic approach for treatment of these illnesses is manipulating the immune system to reduce its activity. In these cases, the therapeutic goal is fine-tuning of the milieu to downgrade the pathological response and return the immune system to a state of controlled homeostasis . However, the modulation of the system has to bring the balance to its normal limits without reducing it beyond these boundaries. It can be compared to adjusting the volume and the tone of music in an orchestra. High volume and distortions reduce the beauty of the music and can cause discomfort. In adjusting the volume and correcting the distortions, the maestro modulates the music, creating a pleasant sensation while still ensuring that each component remains audible.
Figure 1.
You May Like: Long Term Effects Of Psoriasis
Surgery And The Psoriatic Foot
Orthopaedic surgery to correct deformed joints is only justified in the presence of long-standing deformity where pain is preventing adequate mobility and all alternative medical treatments have failed. The advancement of newer techniques in recent years has seen better results in small joint replacement, but such procedures still need careful consideration and discussion with advice from an appropriate surgeon.
What Causes Psoriasis Outbreaks
Psoriasis outbreaks differ from person to person. No one knows exactly what causes flare-ups. Common psoriasis triggers may include:
- Skin injury .
- Streptococcal or other infection that affects the immune system.
- Certain prescription medications .
- Cold weather, when people have less exposure to sunlight and humidity and more to hot, dry indoor air.
Read Also: Blue Star Cream For Psoriasis
Types Of Psoriasis Continued
Examples of other types of psoriasis include:
- Inverse Psoriasis:: This psoriasis may affect skin fold areas such as the genital area, under the breast or arms, or around the groin area. The lesions are flat, red, and often without scales.
- Nail Psoriasis: Nails may become yellow-brown, pitted, flake away or detach from the nail bed.
- Psoriatic Arthritis: May occur in up to 30 percent of patients with psoriasis symptoms include swelling of the knees, ankles, hands and toe joints pain and may be accompanied by nail psoriasis.
Are Psoriasis Shampoos Available
Coal tar shampoos are very useful in controlling psoriasis of the scalp. Using the shampoo daily can be very beneficial adjunctive therapy. There are a variety of over-the-counter shampoos available without a prescription. There is no evidence that one shampoo is superior to another. Generally, the selection of a tar shampoo is simply a matter of personal preference.
Also Check: How To Stop A Psoriasis Flare Up
Appropriate Initial Treatment For Psoriasis Would Be Quizlet
A mother of two living with psoriasis, victoria wants to empower other women this condition and assure them that they are not defined by their psoriasis. With multiple drug classes available for plaque psoriasis treatment, healthcare professionals compare and contrast between the biologic therapies a.
Home Remedies Natural Cures AnhidrosisPlay |
How To Use Corticosteroids Safely
Topical corticosteroids are used to reduce inflammation and are available in different strengths, for example they can be mild, moderate, potent and very potent. Very potent corticosteroids should not be used to treat psoriasis in children or young people. In adults very potent corticosteroids should only be used in specialist care. This treatment needs to be carefully supervised and should only be used for up to 4 weeks.
Potent and very potent corticosteroids should not be used on the face, flexures or genitals.
It is important that you follow the advice given to you about how to use each topical corticosteroid because they can sometimes cause side effects and could even make your psoriasis worse. Your healthcare professional should explain the possible side effects and how to avoid them. If you are using potent or very potent steroids you should have a 4-week break between courses of treatment to prevent you developing side effects. You may be given a different non-steroidal topical treatment to use during this break, such as vitamin D or coal tar.
Recommended Reading: Dr Blaine’s Revitaderm Psoriasis Treatment Reviews
Before Stopping Psoriasis Treatment Talk With Your Dermatologist
Because psoriasis is a lifelong disease, its understandable that you may want to stop treatment at some point. Alwaystalk with your dermatologist before you stop treatment.
Some treatments can be stopped immediately. Others need to be discontinued slowly to prevent psoriasis from worsening .
When psoriasis rebounds, it may become a more serious type of psoriasis. A person who had plaque psoriasis may suddenly have pustular psoriasis or erythrodermic psoriasis.
The best way to prevent a rebound is to talk with your dermatologist. Your dermatologist can tell you whether you can stop the treatment abruptly or slowly. Sometimes, the best approach is to gradually switch to another treatment.
What Does Psoriasis Look Like
Psoriasis can occur on any area of the body, including hands, feet, elbows, scalp or genitals.
- In plaque psoriasis, the most common form of psoriasis, the skin tends to be dry, flaky, itchy, red and covered with white scales.
- Psoriasis can affect small areas of the body or be very widespread.
- For many people, psoriasis can lead to embarrassment, self-consciousness, or stress some people may require treatment for depression or anxiety.
- Family doctors, dermatologists, or rheumatologists may treat your psoriasis depending upon site and severity.
- See more pictures of psoriasis.
Also Check: How Many People Have Plaque Psoriasis
What Will Happen If I Stop Treating My Psoriasis
One of three things happens when you stop treatment:
You may stay clear and have no psoriasis symptoms .
Your psoriasis may return, looking and feeling much like it did before .
The psoriasis may return and be worse than before .
What happens often depends on the medication you were using when you stopped, how well you manage your psoriasis triggers, and your medical history.
Psoralen And Ultraviolet A
Psoralens plus long wave ultraviolet A radiation, , can be applied to the whole body by giving an oral psoralen in tablet form 2 hours prior to treatment.
- Treatment can be localised to the hands and/or feet by using psoralen bath soaks or topical psoralens prior to treatment.
- Localised treatment is commonly used to treat thick plaques or moderate-to-severe hand and/or foot psoriasis, including palmoplantar pustulosis.
- persists for some hours following oral psoralen treatment therefore, patients are advised to avoid sun exposure, including wearing wrap-around sunglasses on the day of treatment.
- PUVA is more likely than narrowband UVB treatment to cause skin cancer, especially squamous cell carcinoma and is usually limited to a maximum of 100 to 200-lifetime treatments.
- Psoralens and therefore PUVA is not recommended during pregnancy or breastfeeding.
Recommended Reading: Psoriasis On Hands Home Remedy
American College Of Rheumatology/national Psoriasis Foundation Guidelines
In 2018, the American College of Rheumatology and the National Psoriasis Foundation developed new guidelines for the treatment of psoriatic arthritis. These guidelines differ from others because it recommends TNFi biologics first for most people.
The ACR/NPF guidelines also suggest treat to target. Your doctor will set a goal and monitor your response to the drugs often, adjusting as needed.1
While everyone is different, the treatments for PsA generally should be tried in this order:1
- Tumor necrosis factor inhibitor biologics such as etanercept, infliximab, adalimumab, golimumab, certolizumab pegol
- Methotrexate, sulfasalazine, leflunomide, cyclosporine, or apremilast
- Interleukin 17i such as secukinumab, ixekizumab, brodalumab
- IL12/23i biologic
The order in which your doctor will try these drugs may change depending on whether you:1
- Severity of the arthritis or psoriasis
- Prefer to take pills over shots
- Have congestive heart failure, serious infections, or certain nerve diseases
- Have severe psoriasis
- Have had a serious reaction to a TNFi biologic
For people with active PsA despite treatment and who also have inflammatory bowel disease , the guidelines recommend trying drugs in this order:1
- TNFi like infliximab, adalimumab, golimumab, or certolizumab pegol
- IL12/23i biologics
For people with active PsA and frequent serious infections who have not tried some of the most common treatments:1
Other non-drug treatments mentioned include:1
Heads Up: Anthralin For Scalp Psoriasis
Anthralin is a prescription topical cream or shampoo for the scalp that slows down the growth of skin cells.
- Anthralin, like coal tar, can be messy, stain fabrics, and has a strong odor.
- Anthralin can also stain the skin or hair with a temporary reddish brown color.
- Treatment may be applied for short periods to help lessen staining and irritation. Follow your healthcare providers instructions for use.
Like coal tar, anthralin may be used in combination with UV light to help with skin symptoms of psoriasis, including dryness, redness, flaking, scaling, and itching.
Recommended Reading: What Is Used To Treat Psoriasis