How Do People Get A Second Type Of Psoriasis On Their Skin
While theres no way to predict who will develop a second type of psoriasis, some people may be more susceptible. For example, having severe psoriasis that isnt well controlled, stopping a strong medication too quickly, or getting strep throat may increase your risk.
The following explains how people who have plaque psoriasis, the most common type of psoriasis, can develop a second type of psoriasis on their skin.
Youll also find out how plaque psoriasis can turn into a different type of psoriasis.
Inverse psoriasis: Many people gain a lot of weight after getting plaque psoriasis. Researchers arent sure why this happens, but they have discovered that extra pounds can increase your risk of developing inverse psoriasis.
Inverse psoriasis only forms in areas where skin touches skin, such as the armpits, groin, or underneath the breasts. It causes smooth, bright-red patches of raw-feeling skin.
Guttate psoriasis: Some people with plaque psoriasis have developed guttate psoriasis after getting an infection, such as strep throat. Guttate psoriasis causes spots on the skin that are small, pink to salmon-colored, and scaly. These spots are often widespread, appearing on the torso, legs, and arms.
Erythrodermic psoriasis: Some people who have severe plaque psoriasis see their plaque psoriasis turn into erythrodermic psoriasis. This can happen when:
Different ways that psoriasis can affect the nails
Occurrence In The United States
According to the National Psoriasis Foundation, psoriatic arthritis affects about 1 million people in the United States, or about 30% of all persons with psoriasis. However, prevalence rates vary widely among studies. In one population-based study, less than 10% of patients with psoriasis developed clinically recognized psoriatic arthritis during a 30-year period. A random telephone survey of 27,220 US residents found a 0.25% prevalence rate for psoriatic arthritis in the general population and an 11% prevalence rate in patients with psoriasis. However, the exact frequency of the disorder in patients with psoriasis remains uncertain, with the estimated rate ranging from 5-30%.
Moreover, since the late 20th century, the incidence of psoriatic arthritis appears to have been rising in both men and women. Reasons for the increase are unknown it may be related to a true change in incidence or to a greater overall awareness of the diagnosis by physicians.
Are People With Psoriatic Arthritis At Greater Risk For Covid
This is an ongoing area of research.
The National Psoriasis Foundations guidance says that it is not known with certainty if having psoriatic disease meaningfully alters the risks of contracting SARS-CoV-2 or having a worse course of COVID-19 illness. It notes that existing data, with some exceptions, generally suggest that patients with psoriasis and/or psoriatic arthritis have similar rates of SARS-CoV-2 infection and COVID-19 outcomes as the general population.
The ACRs guidance says that autoimmune and inflammatory rheumatic disease patients are at higher risk for being hospitalized due to COVID-19 and having worse outcomes compared to the general population.
However, this is likely affected by factors such as age, other comorbidities such as heart disease or obesity, which is common in PsA, and taking steroid medications, rather than simply having psoriatic arthritis alone.
Some data suggests that patients with inflammatory rheumatologic diseases who get COVID-19 may have higher risk of developing serious complications, depending on their disease activity and other medical conditions such as high blood pressure, diabetes, and chronic kidney and lung disease, adds Dr. Zhu.
For more information, check out this summary of research on inflammatory arthritis and rheumatic disease patients and their risk for COVID-19 complications.
Also Check: Can Psoriasis Spread To Face
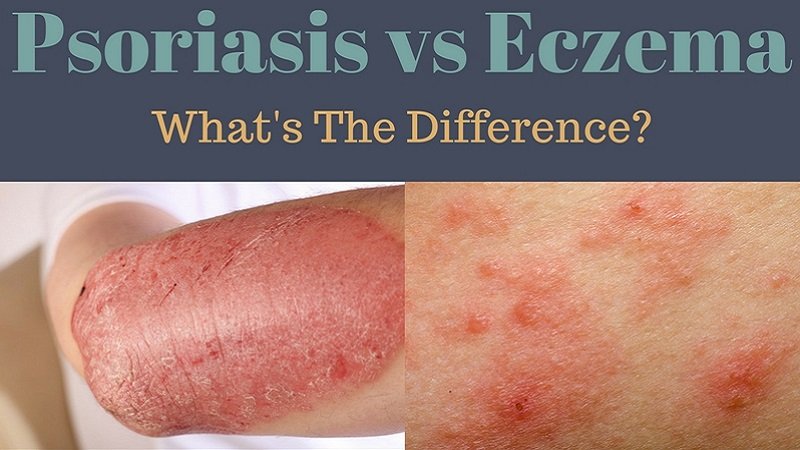
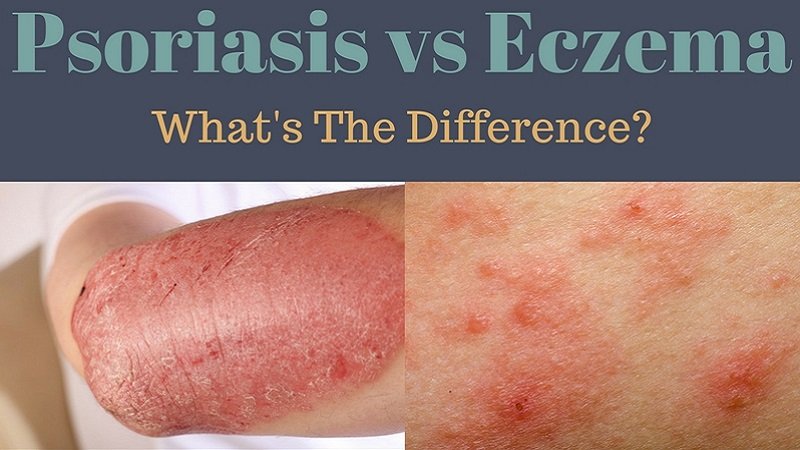
What Is Atopic Dermatitis Or Eczema
Atopic eczema is a common skin condition that is characterized by dry, itchy, and scaly patches. Atopic eczema is known for the intense itching that it causes. Atopic eczema most often occurs in children, with 90% of all cases being diagnosed before the age of 5.4,5 As a chronic condition, atopic eczema may have periods of remission and periods of flares. Atopic eczema may also appear differently depending on the age of the person affected. A primary care doctor or dermatologist will inspect the skin and asks about symptoms that you are experiencing such as itch. Sometimes, a provider may conduct a patch test to determine if you have skin allergies.
What Is Erythrodermic Psoriasis
Erythrodermic psoriasis is a rare form of psoriasis associated with extreme inflammation, itching and pain that affects most of the body. Other symptoms include large sheets of shedding skin , an increase in heart rate, swelling due to fluid retention and significant changes in your body temperature. Its important to seek immediate medical attention if youâre experiencing a flare-up of erythrodermic psoriasis as it can lead to pneumonia or heart failure if left untreated.6
Also Check: Natural Shampoo For Scalp Psoriasis
Though Psoriasis And Eczema Are Different Conditions Treatment For The Two Is Often Similar
While theres no cure for either condition, they can be treated. If youre diagnosed with psoriasis or eczema, your doctor may recommend:
- Over-the-counter moisturizers
- Topical medications to reduce inflammation, like corticosteroids, calcineurin inhibitors, and retinoids
- Oral steroids, like prednisone, which can help calm a severe case when used for a short period of time
- Wet dressings, which involve wrapping the area with a wet bandage to soothe the itchiness
Although psoriasis and eczema are both frustrating, irritating conditions, they shouldnt be life-ruiners. If youre struggling with managing your psoriasis or eczema, see a dermatologist, who can help determine the best treatment plan for you.
Related:
How To Tell Seborrheic Dermatitis From Psoriasis
To tell the two apart, youâll need to take a close look at the differences in those patches, or plaques. Psoriasis starts as rough, red, scaly skin and grows into thick, usually silver-colored scales on top of those areas. These patches often show up on the scalp. You can also get them on your torso, limbs, hands, and feet.
Seborrheic dermatitis patches are more likely to vary in color. They may look whitish-yellow, red, or brown. They also tend to feel greasy or oily . This form of dermatitis, or inflammation of the skin, strikes most often on the scalp, on oily parts of the face , and on the upper chest and back. Think of it as dandruff 2.0. Simple dandruff causes only flakes, no inflammation, and itâs only on the scalp.
Itâs tricky to figure out which condition is which when the flaky red patches are only on the scalp, with no other clues. Itâs also possible to have both conditions at the same time. Thatâs called sebopsoriasis, and it can leave you with white and silver flakes.
Recommended Reading: Best Hair Grease For Psoriasis
How Are Ra And Psa Diagnosed
Because these two conditions share similar symptoms, itâs important to get an accurate diagnosis from a rheumatologist. A rheumatoid factor blood test is one way your doctor can tell which condition you have. RF is a protein found in people with rheumatoid arthritis. People with PsA usually donât have it. Blood tests looking for other antibodies such as anti-CCP can also help differentiate the two.
Another way to tell is to look at your skin and nails. If you have scaly patches on your skin, pitting and flaking on your nails, or both, you have PsA.
Once youâve had the disease for a while, X-rays might also be able to distinguish the two conditions.
It is possible to have RA and PsA together, but itâs rare. If you do have both, many of the treatments, including some medications, will work for both conditions.
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
Recommended Reading: Can Rheumatoid Arthritis Affect Your Lungs
Read Also: Can Scalp Psoriasis Cause Headaches
How Is Psoriasis Treated
The type of psoriasis and the severity of the individual’s psoriasis will help to determine what course of treatment will be appropriate. There are a variety of topical treatments that may help improve symptoms of psoriasis, including topical corticosteroids. Other ways to manage and treat psoriasis symptoms include light therapy , systemic treatments, biologics, other medications, lifestyle modifications or alternative and complementary therapies.3
Summary Plaque Psoriasis Vs Psoriasis
Psoriasis is a chronic multisystem disease with skin and joint manifestations. Plaque psoriasis is the commonest form of psoriasis which is characterized by the appearance of reddish well-demarcated plaques with silver scales usually on the extensor surface of the knees and elbows. Accordingly plaque psoriasis is one manifestation of the broad spectrum of dermatological and systemic manifestations which are identified as psoriasis. This can be identified as the difference between plaque psoriasis and psoriasis.
Also Check: What Is The Best Treatment For Guttate Psoriasis
Where Did It Appear
Eczema and psoriasis both can appear on any part of the body. However, both conditions have areas where breakouts are predominant.
Eczema breakouts tend to appear on the areas of the body that bend like behind the knees and inside elbows. It can also be on your ankles, wrist, and neck. Babies may have it nearly anywhere on their bodies.
Psoriasis may also appear all over the body however, there are areas where it tends to appear that eczema doesnt, including:
- Soles of the feet and palms of the hand
- Fingernails and toenails
- Eyelids
- Mouth and lips
If your rash is in these areas, that is a good indicator that you are dealing with psoriasis and not eczema.
What Are The Symptoms Of Psoriasis

There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
You May Like: Psoriasis Treatment In Ayurveda Patanjali
Read Also: Early Signs Of Scalp Psoriasis
When Did It Start
One factor that helps a dermatologist tell the difference in psoriasis, eczema is determining the age of people at the onset of the skin condition. Eczema normally appears in infants and continues through adulthood. On the other hand, psoriasis typically appears in the late teens to early twenties but can appear in children.
What Are The Types Of Psoriasis
In children, common types of psoriasis include:
Plaque psoriasis. This is the most common type of psoriasis. It causes plaques and silvery scales, usually on the knees, elbows, lower back, and scalp. They can be itchy and painful and may crack and bleed.
Guttate psoriasis. This type often shows up after an illness, especially strep throat. It causes small red spots, usually on the trunk, arms, and legs. Spots also can appear on the face, scalp, and ears.
Inverse psoriasis. This causes smooth, raw-looking patches of red skin that feel sore. The patches develop in places where skin touches skin, such as the armpits, buttocks, upper eyelids, groin and genitals, or under a womans breasts.
Read Also: O Keeffeâs For Eczema
Also Check: Is Manuka Honey Good For Psoriasis
What Is The Link Between The Conditions
People with psoriatic arthritis often also have psoriasis, says Dr. Mhlaba. But just because you have psoriasis does not mean you have psoriatic arthritis.
Both psoriasis and psoriatic arthritis can lead to pain, discomfort and even embarrassment. You may have trouble doing daily tasks, especially those that involve fine motor skills.
In addition, the severity of the conditions is not always the same. Your psoriasis might be severe when your psoriatic arthritis is mild, and vice versa. The unpredictable natures of these conditions can be hard to manage on your own. Given this, Dr. Mhlaba recommends a group approach to treatment.
“Psoriasis and psoriatic arthritis are best managed by a team,” she says. “Most often, this would consist of a dermatologist, a rheumatologist and a primary care physician.”
If you have questions about your skin or think you have psoriasis or another skin issue, see your dermatologist or primary care physician. They can make a diagnosis and recommend the best treatment.
Related Services
Understanding Psoriasis And Predisposition
While we know psoriasis is caused by the immune system, the exact cause is not known. The same can be said for psoriatic arthritis. Statistically, about 40 percent of people with psoriatic arthritis have relatives with psoriatic arthritis or with psoriasis, but scientists do not know what genes lead to these conditions. Ongoing research is investigating the causes of psoriasis and psoriatic arthritis in order to predict who may develop these conditions and to invent new treatments.
Also Check: Is Egg Good For Psoriasis
What Is Psoriatic Arthritis
Psoriatic arthritis is a form of arthritis that affects roughly 30% of people with psoriasis. The condition is characterized by joint inflammation.
Other symptoms can include:
- Inflamed, swollen and painful joints, usually in the fingers and toes
- Deformed joints from chronic inflammation
These symptoms closely mirror other types of arthritis. However, psoriatic arthritis is easier to diagnose if you already have psoriasis.
They Have Different Causes
Psoriasis and eczema have different causes.
- Psoriasis is an autoimmune disease, which means that its caused by an overactive immune system. Doctors still dont know what causes the immune system to behave this way. Those with psoriasis shed skin cells at a much quicker rate than normal. As dead skin cells build up, they cause psoriasis plaques.
- Eczema is a skin condition thats caused by certain triggers. These triggers cause inflammation in the body and the immune system to overreact. Eczema can be triggered by a variety of things, from allergies to stress, cold weather and even fragrances.
Psoriasis may also be triggered by many of the same things that trigger eczema, but injuries and medications can also cause flare-ups. In addition, many people with psoriasis are sensitive to heat, and their symptoms may get worse in the summer.
Don’t Miss: What Makes Psoriasis Flare Up
Is There A Cure For Psoriasis
There is no cure at the moment. However, as a consequence of current research, our understanding about what happens in psoriasis is growing and new drugs are being developed. In the meantime, there are a number of treatments that are effective in keeping psoriasis under control.
The art of treating psoriasis is finding the best form of treatment for each individual. There is no single solution that is right for everyone.
Approach To The Patient
Evidence-based guidelines35 on the treatment of patients with chronic plaque psoriasis were published in 2004 by the Finnish Dermatological Society. Recommendations for the management of psoriasis in primary care, based on these guidelines, the evidence cited above, and considering common practice among American dermatologists, are shown in Figure 9.35
Management of Chronic Plaque Psoriasis
Figure 9
Algorithm for the management of chronic plaque psoriasis, based on recent guidelines,35 current evidence, and common practice among American dermatologists.
Management of Chronic Plaque Psoriasis
Figure 9
Algorithm for the management of chronic plaque psoriasis, based on recent guidelines,35 current evidence, and common practice among American dermatologists.
For the initial treatment of psoriasis on limited areas of skin, the most effective treatment is a combination of potent topical steroids and calcipotriene. This recommendation, however, is based on limited evidence.18,29,30 An alternative would be to start with a potent topical steroid, calcipotriene, or a topical retinoid alone. Calcipotriene and topical retinoids can be used long-term, but topical steroids must be used intermittently because of their side effects.35
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.
Read Also: Does Psoriasis Make You Heal Faster
Psoriatic Arthritis: What Is The Connection
Psoriatic arthritis : 1 in 4 of people with psoriasis may develop an associated arthritis called psoriatic arthropathy, which causes pain and swelling in the joints and connective tissue, accompanied by stiffness particularly in the mornings and when rising from a seat. Most commonly affected sites are the hands, feet, lower back, neck and knees, with movement in these areas becoming severely limited. Chronic fatigue is a common complaint linked with this condition. If you are experiencing mild aches and pains and have psoriasis, even very mildly, consult your dermatologist for further advice and if necessary a referral to a rheumatologist for further assessments. For more detailed information on psoriatic arthritis see What is Psoriatic Arthritis?