Does Psoriasis Weaken The Immune System
Psoriasis skin lesions are thought to be the result of an overactive immune response.
With psoriasis, the body produces too many inflammatory agents, called cytokines, which normally help fight infections and heal injuries. But instead of focusing on fighting off an infection or injury, these cytokines also attack healthy tissue.
Psoriasis itself doesnt weaken the immune system, but its a sign that the immune system isnt working the way it should. Anything that triggers the immune system can cause psoriasis to flare up. Common ailments like ear or respiratory infections can cause psoriasis to flare.
Many people with psoriasis are prescribed immunosuppressive drugs to manage the condition. Because these drugs suppress the immune system, they increase your risk for contracting viruses like a cold and the flu. If you do get sick, these illnesses may last longer than they would if you didnt take these medications.
Talk with your healthcare provider about ways to stay healthy. That includes getting an annual flu vaccine, washing your hands regularly, and adjusting your treatment plan if you do get sick.
What Does It Look Like
Hypereosinophilic syndrome usually presents with fever, weight loss, fatigue, and rash.
A rash is present in over 50% of patients, but is non-specific in appearance. Most commonly, red swollen itchy nodules have been described. It can also resemble urticaria .
An enlarged liver and spleen is often present indicating liver and spleen involvement. The lungs, kidneys, heart and nervous system can be affected.
Hypereosinophilic syndrome
Hronic Spongiotic Dermatitis Treatment
Clinical psoriasiform dermatitis developed in our patient after treatment with dupilumab for autoeczematization secondary to chronic stasis dermatitis. Similar events have been reported in patients with atopic dermatitis who developed psoriasiform dermatitis after treatment with dupilumab, but this is the first case related to. Acute Spongiotic Dermatitis. The term ‘eczema’ derives from the Greek ekzein ‘to boil over,’ reflecting the clinical appearance of acute lesions. Clinically, it exhibits erythematous macules, papules, and plaques .With increasing degrees of spongiosis, lesions become vesicular or bullous and begin to weep or to ooze L30.8 is a billable diagnosis code used to specify a medical diagnosis of other specified dermatitis. The code L30.8 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions. The ICD-10-CM code L30.8 might also be used to specify conditions or terms like acneiform.
Also Check: Why Do I Only Have Psoriasis On My Scalp
Lichenoid Granulomatous Dermatitis Revisited: A
T1 – Pretibial pruritic papular dermatitis. T2 – A distinctive cutaneous manifestation in response to chronic rubbing. AU – Annessi, Giorgio. AU – Petresca, Marsilia. AU – Petresca, Angela. PY – 2006/4. Y1 – 2006/4. N2 – We describe the clinico-pathologic features of 44 patients with a peculiar pretibial pruritic papular dermatitis These include psoriasis 58 , seborrheic dermatitis, psoriasiform drug eruption, chronic fungal infections, lichen simplex chronicus, chronic spongiotic dermatitis, Psoriasiform dermatitis Table 4 Epidermal changes in psoriasiform dermatoses Table 5 Dermal changes in psoriasiform dermatitis This type of inflammatory. Neutrophilic spongiosis is characterized by the presence of neutrophils within spongiotic foci in the epidermis . The term spongiform pustular dermatitis can be used for a severe form of neutrophilic spongiosis in which pustules can be seen clinically and histologically. Subcorneal pustules are excluded from this category
Hypereosinophilia In Erythrodermic Psoriasis: Superimposed Scabies
Cutis
From Dicle University, Diyarbakr, Turkey. Drs. Harman, Uçmak, and Akkurt are from the Department of Dermatology, and Dr. Türkçü is from the Department of Pathology.
The authors report no conflict on interest.
Correspondence: Mehmet Harman, MD, Dicle Üniversitesi Tp Fakültesi, Dermatoloji Anabilim Dal, 21280 Diyarbakr, Turkey .
Scabies is a common ectoparasitic disease that can be diagnosed based on the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. If a desquamative disease such as psoriasis precedes scabies, then the disease course may be altered. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis. We present 2 cases of scabies in a brother and sister with erythrodermic psoriasis. In both cases peripheral hypereosinophilia suggested scabies. In patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents, peripheral eosinophilia also could suggest scabies therefore, a search for sarcoptic mites in skin scrapings should be undertaken.
Don’t Miss: Laser Treatment For Nail Psoriasis
Learn More About Your High Absolute Eosinophil Count
A high absolute eosinophil count can be used to confirm the diagnosis of an infection, certain disorders, or a disease. If you have symptoms of any of the conditions listed above, a physician may order an absolute eosinophil test to confirm the diagnosis.
For the fastest diagnosis without having to make an appointment, visit your local FastMed Urgent Care clinic. Our state-of-the-art facilities include on-site labs where your blood sample can be evaluated for eosinophil levels, as well as for any other blood disorders.
We are open 365 days a year and offer extended weekday hours for your convenience. Contact us with any additional questions you have, and check out what some of our patients have to say about their experience at FastMed Urgent Care:
The professionals at the urgent care center are courteous, as well as speedy. The facility is very clean and inviting. I have been to the medical center a few times, and have sent friends there. No ones ever been disappointed. Mary H.T.
–
Can Psoriasis Kill You
Although psoriasis isnt considered to be a terminal condition, a 2017 study found that people with psoriasis that covered at least 10 percent of their body had 1.79 times greater risk for death in comparison to the general population.
Findings also showed that these people with more severe psoriasis had a greater risk for developing other serious, potentially life threatening conditions. Those include:
- chronic kidney disease
- cardiovascular disease
- diabetes
The study authors concluded that individuals with high surface area psoriasis should be screened for health prevention measures in order to help close the mortality gap.
, people with psoriasis may also have a greater risk for developing an autoimmune condition, such as:
- vitiligo
- thyroiditis
- rheumatoid arthritis
Whether psoriasis itself is an autoimmune condition has yet to be proven. But its considered to be a T-cell mediated disorder of immune dysregulation.
Not everyone with psoriasis will be diagnosed with an additional inflammatory- or autoimmune-related health condition. But the risk for developing one does increase when youre diagnosed with psoriasis.
If you have psoriasis, you may want to discuss your risk for these comorbid conditions with your healthcare provider.
Don’t Miss: What Is The Best Steroid Cream For Psoriasis
Products Of Collagen Degradation
Fragments released as a result of type I and type II collagen degradation including C-terminal telopeptide of collagen I and CTXII, collagen type II degradation product epitopes C2C and C1,2C as well as matrix proteins such as cartilage oligomatrix protein are reflective of bone and cartilage damage. Several studies have investigated the association of these molecules with radiographic progression in early RA patients. Three authors reported that elevated levels of CTXI and CTXII are associated with long-term radiographic progression in early RA patients . What is more, Garnero and colleagues reported that CTXI and CTXII were even more predictive of joint damage compared with CRP and ESR . Bakker and colleagues found that elevated baseline levels of C1,2C were associated with radiographic progression after 1 year of treatment . Additionally Verstappen and colleagues demonstrated that C2C significantly correlated with radiographic progression after 1 year and importantly remained predictive the following year . Andersson and colleagues demonstrated that increments in COMP levels during a 3-month period following diagnosis were predictive of joint damage at 1-year, 2-year and 5-year follow-up . The culmination of positive findings makes these degradation products attractive candidates for a biomarker panel predictive of joint damage.
Possible Eosinophil Effector Functions In Autoimmune Diseases
Eosinophils are extremely versatile effector cells that damage tissues or modulate the activity of other immune and stromal cells. One could envision many of these effector functions playing a role in the context of autoimmune diseases as well . Damage of tissues and cells is a feature of many organ-specific autoimmune diseases. Eosinophils are well known for their strong cytotoxic properties, mediated mostly through granule proteins. This could contribute to organ destruction in autoimmune inflammation.
Box 1. Possible eosinophil effector functions in autoimmune diseases.
Damage of tissues by cytotoxic granule proteins
Antibody-dependent cellular cytotoxicity
Activation of tissue remodeling and fibrosis
Antigen presentation
Modulation of the adaptive immune response
Promotion of B cell responses
Induction of tissue repair processes.
The ability of eosinophils to bind antibodies and consequently degranulate and kill cells links the adaptive autoimmune response to eosinophil effector functions. Eosinophils express complement receptors and Fc receptors either constitutively or under inflammatory conditions . As a result, they are capable of antibody-dependent cellular cytotoxicity to parasites and mammalian targets . In autoimmune diseases, eosinophils may kill host cells bound by autoantibodies.
Read Also: Wet Wrap Therapy For Psoriasis
Enzyme Mediators Of Destruction
The association of matrix metalloproteinase , proteases that promote cartilage breakdown, with joint damage has also been investigated. Previous early RA cohort studies demonstrated that elevated levels of MMP-3 at baseline correlate significantly with radiographic progression . However, another study documented that serial, longitudinal measurements of MMP-3 fail to correlate with measures of joint damage . It can thus be speculated that MMP-3 may be a useful predictive marker of joint destruction at disease onset prior to treatment. MMP-1 might also have prognostic utility and its association with joint damage has been assessed. Previously, elevated baseline levels of MMP-1 were demonstrated to significantly correlate with radiographic progression observed at 12 months . It has also been reported that serial measurements of MMP-1 over a period of 18 months correlate significantly with measures of joint damage . In contrast, Young-Min and colleagues found no correlation between levels of MMP-1 and joint damage in early RA patients . It is certainly possible that differences in study design and data analysis gave rise to these discrepancies, and the relationship between MMP-1 and joint damage warrants further investigation.
Psoriasiform Spongiotic Dermatitis Bmj Case Report
- ent feature of the disorder
- Dermatitis Definition Dermatitis is a general term used to describe inflammation of the skin. Description Most types of dermatitis are characterized by an itchy pink or red rash. Contact dermatitis is an allergic reaction to something that irritates the skin and is manifested by one or more lines of red, swollen, blistered skin that may itch or seep. It.
- Extensive spongiosis, initially acute spongiotic dermatitis, evolving into subacute or chronic spongiotic dermatitis, which then resolves May have intraepidermal vesicles, exocytosis, papillary dermal edema or perivascular lymphocytic infiltrates in upper dermis, also numerous eosinophils
Also Check: Natural Ways To Treat Scalp Psoriasis
What The Test Does
The eosinophil count measures the amount of eosinophils in your blood.
The key is for eosinophils to do their job and then go away. But if you have too many eosinophils in your body for a long time, doctors call this eosinophilia. It can cause chronic inflammation, which could damage tissues.
Conditions where too many eosinophils are in the body include eosinophilic esophagitis and eosinophilic colitis . Eosinophilic disorders also can happen in your stomach, small intestine, blood, or other organs. Sometimes, a biopsy will show that you have a high amount of eosinophils in your tissues, but you might not have a high amount in your blood.
Continued
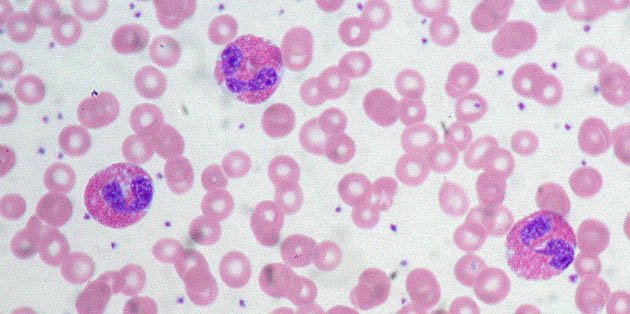
Eosinophils And White Blood Cells

Bone marrow produces five types of white blood cells, all of which are vital components of the immune system. The bone marrow produces more white blood cells when the immune system senses an invasion from a harmful allergen, parasite, virus, or bacteria.
Each type of white blood cell attacks a different infection or allergen. Elevated levels of any of these cells indicates that the body has mounted an attack on an invading infection.
Eosinophils perform two important functions in the immune system. Eosinophils destroy foreign substances that the immune system has identified as dangerous to the body. They also promote inflammation that isolates and controls a disease or infection site.
Read Also: Safe Psoriasis Treatment While Pregnant
Eosinophilic Granulomatosis With Polyangiitis
Eosinophilic granulomatosis with polyangiitis was first described by Churg and Strauss in 1951 . The disease progresses through three overlapping phases: adult-onset asthma, peripheral and tissue eosinophilia, and necrotizing vasculitis with tissue infiltration of eosinophils . EGPA is an idiopathic type of small vessel vasculitis and is also part of the hypereosinophilic syndromes . It is associated with HLA and IL-10 polymorphisms . About 40% of EGPA patients have perinuclear ANCA antibodies against myeloperoxidase , resulting in the classification of EGPA as an ANCA-associated vasculitis . The presence or absence of ANCA in EGPA may indicate two clinical subtypes with different organ involvement. ANCA-positive patients have more frequent vasculitis and glomerulonephritis, whereas ANCA-negative patients have more frequent heart and lung involvement .
Blood eosinophils in EGPA show an activated phenotype expressing high levels of CD69 and CD11b . Moreover, they express IL-25, a cytokine that increases release of IL-4, -5, and -13 from T cells. Serum IL-25 is increased in patients with active EGPA compared to inactive disease or healthy controls. It is also detectable in eosinophils from lesional biopsies. T cells in these biopsies and in the blood express the IL-25 receptor IL-17RB . This suggests a feed-forward loop between eosinophils and Th2 cells in EGPA.
Related Publications That Referenced Our Studies
- Guidelli GM, Tenti S, Fioravanti A, “Severe eosinophilia during anti-tumor necrosis factor-alpha therapy for psoriatic arthritis”, Indian Journal of Dermatology, Venereology, and Leprology, 2015 Jan .
- Malisiewicz B, Murer C, Schmid JP, French LE, Schmid-Grendelmeier P, Navarini AA, “Eosinophilia during psoriasis treatment with TNF antagonists”, Dermatology, 2013 Jan .
Also Check: Essential Oil Treatment For Psoriasis
Severe Eosinophilia During Anti
Correspondence Address
| How to cite this article: Guidelli GM, Tenti S, Fioravanti A. Severe eosinophilia during anti-tumor necrosis factor-alpha therapy for psoriatic arthritis. Indian J Dermatol Venereol Leprol 2014 80:187-189 |
Sir,
Since 1999, tumor necrosis factor-alpha antagonists are being commonly used in the treatment of rheumatological, dermatological and gastroenterological autoimmune diseases.
Despite their striking effectiveness and an acceptable toxicity profile, several side effects have been reported, including increased risk of serious infections due to both commensal and opportunistic microorganisms, lymphoma and solid tumors and adverse dermatological reactions.
Here, we briefly report the case of a man with psoriatic arthritis who developed blood eosinophilia first during treatment with etanercept and then with adalimumab.
A 59-year-old Caucasian man had been diagnosed with psoriatic arthritis 15 years ago. Initially, during the early years of the disease, he reported being treated with oral corticosteroids and sulfasalazine and then with methotrexate.
| Figure 1: Variation in eosinophil counts over time |
After 6 months of treatment with oral corticosteroids alone, the patient was seen in our rheumatologic outpatient clinic for a relapse of the arthritis. Clinically, the patient showed joint effusion of his right knee, wrists and small joints of the left hand psoriasis plaques were still present on his elbows .
Vulvar Inflammatory Dermatoses For The Non
Lymphoeosinophilic infiltrates are found in a number of disorders including subtypes of dermatitis, insect bite reactions, autoimmune bullous diseases and drug reactions. 1 Eosinophilia, both peripheral and in cutaneous tissue, is not a common finding in mycosis fungoides however, it has been described in association with folliculotropic mycosis fungoides and tumor stage MF For instance perivascular dermatitis with eosinophils too many white cells will cause autoimmune symptoms and conditions. Superficial and deep perivascular dermatitis falls under inflammatory skin diseases that a dermatologist will diagnose for you. . Perivascular dermatitis can be divided into four types Article. Psoriasiform spongiotic dermatitis. March 2019 BMJ Case Reports 12:e22869 Clinicians who diagnose lichenoid granulomatous dermatitis may wish to look for dermal eosinophilia, psoriasiform epidermal changes, periadnexal inflammation, and red blood cell extravasation in an effort to improve diagnosis of this condition, a study in the Journal of the American Academy of Dermatology reports.. A total of 56 cases of LGD were collected from 3 different laboratory. The inflammatory dermatoses with epidermal changes are classified histologically into spongiotic dermatitis, interface dermatitis, and psoriasiform dermatitis. Spongiotic dermatitis. Spongiotic dermatitis is defined by the presence of epithelial intercellular oedema. 32 It is caused by a variety o
Read Also: Early Signs Of Scalp Psoriasis
What Is Hypereosinophilic Syndrome
Hypereosinophilic syndrome is a rare condition defined by three criteria:
The condition largely occurs in males , typically at middle age.
Some patients have an underlying blood disorder present, most commonly a form of leukaemia. Leukaemia may also be diagnosed up to 9-12 years after the initial diagnosis of hypereosinophilic syndrome.
Histological Patterns And Differential Diagnosis Of Common
You May Like: Is Psoriasis And Psoriatic Arthritis Related