What Is The Cause Of Palmoplantar Pustulosis
The exact cause of palmoplantar pustulosis is unknown. There have been several theories.
- It may be a disorder of the eccrine sweat glands, which are most numerous on palms and soles.
- Genetic factors are important as several members of some families are affected. Some cases have been associated with IL36RN genemutations
- It may be autoimmune and autoinflammatory in origin.
- Some cases are drug-induced and are especially reported in patients on tumour necrosis factor alpha inhibitors.
The majority of patients with palmoplantar pustulosis are current smokers and in those that have smoked in the past . It is thought that activated nicotine receptors in the sweat glands cause an inflammatory process.
Clinical Manifestations And Imaging
SAPHO syndrome is characterized by the combination of skin and osteoarticular manifestations. The skin manifestations include palmoplantar pustulosis, severe acne, suppurative hidradenitis, and at times psoriasis. The skin manifestations can precede or follow the osteoarticular manifestations, at times by many years.117,126,127
The osteoarticular features of SAPHO syndrome are hyperostosis, aseptic osteitis that occasionally involves the adjacent joints, and synovitis. The early histologic findings of the bone lesions are similar to those of osteomyelitis with periosteal bone formation. Subsequently the lesions evolve into chronic inflammation with a preponderance of mononuclear infiltrate it is only in the late phases that prominent marrow fibrosis, sclerosis, and enlarged bone trabeculae ensue.128
Laboratory investigations may reveal a moderately elevated erythrocyte sedimentation rate or acute phase reactants such as C-reactive protein, C3, and C4. These findings may reflect the inflammatory nature of the condition but are less reliable than in other inflammatory rheumatic disorders.117,125
Dermatologic Adverse Reactions During Anti
Mocci G, Marzo M, Papa A, Armuzzi A, Guidi L. J Crohns Colitis 2013 7: 76979.
Review about the potential skin side effects of anti-TNF blockade, including psoriasiform lesions and PPP.
Benefit of TNF- antagonist use in PPP is conflicting, with therapeutic efficacy, PPP initiation, or aggravation occurring.
Also Check: Light Therapy Lamp For Psoriasis
Treating A Patient With Blisters And Papules On The Soles
A 29-year-old Caucasian female patient presented in consultation in the foot and ankle clinic regarding a six-week history of erythematous vesicles and papules on the soles. She reported intense pruritus. Her primary care physician told her that she had a case of athletes feet and that she should use an over-the-counter antifungal cream. After two weeks of treatment with antifungal cream, the patient had no improvement. The Which Oil Best For Eczema
Types Of Pustular Psoriasis
Generalized pustular psoriasis is a chronic and relapsing condition that presents with a sudden onset of rash and pustules located on nonacral skin. Generalized pustular psoriasis also commonly presents with systemic symptoms, including fever, pain, and malaise, the severity of which vary case-by-case, as well as psoriasis vulgaris. However, the presence of systemic inflammation and psoriasis vulgaris are not necessary for diagnosis.
The annular type is also known as subacute generalized pustular psoriasis. It tends to run a subacute or chronic course with fewer systemic manifestations. A disproportionately high number of cases are found in the pediatric population.
Palmoplantar pustulosis is a localized form of pustular psoriasis and presents with chronic pustular eruptions of the palms and soles. Palmoplantar pustulosis is not typically associated with the life-threatening complications seen in generalized pustular psoriasis however, possible complications include skeletal and joint disease.
Acrodermatitis continua of Hallopeau is a chronic form of pustular psoriasis characterized by pustular eruptions of the tips of the fingers and toes, which spare the underlying joints and bone. Cases are generally refractory to treatment. Subsets of these cases are considered variants of pustular psoriasis, particularly since they are indistinguishable histologically and in early clinical presentation.
Don’t Miss: Natural Remedies For Psoriasis On Head
Things You Can Do To Ease Pompholyx
You should try to avoid contact with anything that might irritate your skin, including soaps, shampoos and other household chemicals.
Use an emollient as a soap substitute and wear cotton-lined gloves when youre at risk of contact with other potentially irritating substances, such as when washing your hair or doing housework.
Do not burst the blisters. Let them heal on their own. If theyre particularly big, your GP may be able to drain them.
Targeted Therapies Approved For Psoriasis Vulgaris
Biological agents have changed the therapeutic approach to severe and refractory cases of psoriasis.9 However, the high associated costs and possible adverse events related to immunomodulation/immunosuppression of these drugs have forced the necessity to apply criteria for their prescription.9 Most Phase 2 and 3 controlled and randomized studies for approval and verification of the safety of these molecules excluded patients with PPP. The exclusion occurs due to undefined criteria in the literature as well as these patients generally not achieving sufficiently high values in the area of psoriasis and severity index and/or BSA to meet the criteria for inclusion of trials. Thus, data concerning the efficacy of biological agents in PPP are rare and are restricted to a low number of clinical reports and isolated clinical trials. It is important to emphasize that biological are symptomatic treatments, and as so, they do not affect the course of the disease.
TNF Inhibitors
IL-12/23 Inhibitors
Ustekinumab, a drug that targets the p40 subunit common to IL-23 and IL-12, has exhibited conflicting results in PPP patients. It may be effective in some cases refractory to treatment with TNF-a inhibitors.76
IL-17 Inhibitors
IL-23 Inhibitors
Phosphodiesterase-4 Inhibitor
Don’t Miss: What Is The Best Remedy For Psoriasis
Diagnosis Of Palmoplantar Pustulosis
To see if you have PPP, your doctor will check your skin. Most often, they’ll take a painless scrape or swab of the area.
Sometimes, they’ll need to remove a small piece of skin to confirm PPP. The area will be numbed, and you may need a few stitches afterward. Your doctor will look at the tissue under a microscope to see if you have PPP.
Treatment Of Eczema Vs Psoriasis
Both eczema and psoriasis are treated by modulating the immune system. Topical Corticosteroids are commonly used to treat both conditions. The effects of topical medications are mostly limited to the skin. In severe cases of eczema, it may be necessary to take systemic oral medications such as Methotrexate or Mycophenolate mofetil.Read more about eczema treatments.
Since psoriasis is a chronic autoimmune disease that can cause systemic symptoms and progressive joint damage, it is important to calm the immune system throughout the body to control inflammation and reduce autoimmune attacks on the skin and joints. Systemic treatments for psoriasis include immunomodulators such as Methotrexate and newer biologic drugs such as Enbrel , Humira , and Stelara , which are injected.
, or light therapy, may also be helpful in some cases of psoriasis or eczema.
Condition Guide
FAQs
Whats the difference between hives and eczema?Hives can be similar in appearance to eczema, with itchy red patches of skin on different parts of the body. However, hives are generally smoother in appearance and quickly disappear. Hives rarely bleed, and the onset can be sudden. Hives may occur once, may last for a short period over time or over months, or may be chronic. Hives are usually caused by an allergy.
Is there an eczema and psoriasis cream?There are several topical medications such as lotions, creams, and ointments that may be prescribed for either eczema or psoriasis.
Read Also: Eczema And Psoriasis Body Wash
Treatment Options For Dyshidrotic Eczema
That doesnt mean patients should throw up their hands and give up. The most important step is to get a proper diagnosis.
Dyshidrotic eczema can mimic contact dermatitis and even palmoplantar pustulosis, a type of psoriasis appearing on the hands and feet, said Siegfried. The only way to tell which is which is with a biopsy. Without a definitive diagnosis, patients could receive suboptimal treatment.
On the positive side of the line, people with the condition have several options. In addition to avoiding triggers, Siegfried pointed to the following treatments and their limitations. Topical corticosteroid cream can be helpful as a quick-acting remedy, she said.
Think of it as the hare in the fable of The Tortoise and the Hare. It may get quick results, but it can also weaken the skin over time, leading to a cycle of flare and remission.Its best to switch to another therapy after a couple of weeks, such as a topical calcineurin inhibitor or phototherapy.
Over the years, Wanamaker has tried all these and more. Her grandmother used to create a paste from cornstarch and water and apply it to her young granddaughters handsa home remedy that brought short-term relief for her itchy skin.
And theyre hopeful that better treatments are on the way. Were at the dawn of the decade of eczema, as Siegfried sees it. With all the medications in the pipeline for AD, can dyshidrotic eczema be far behind?
Localized Pustular Psoriasis Variants
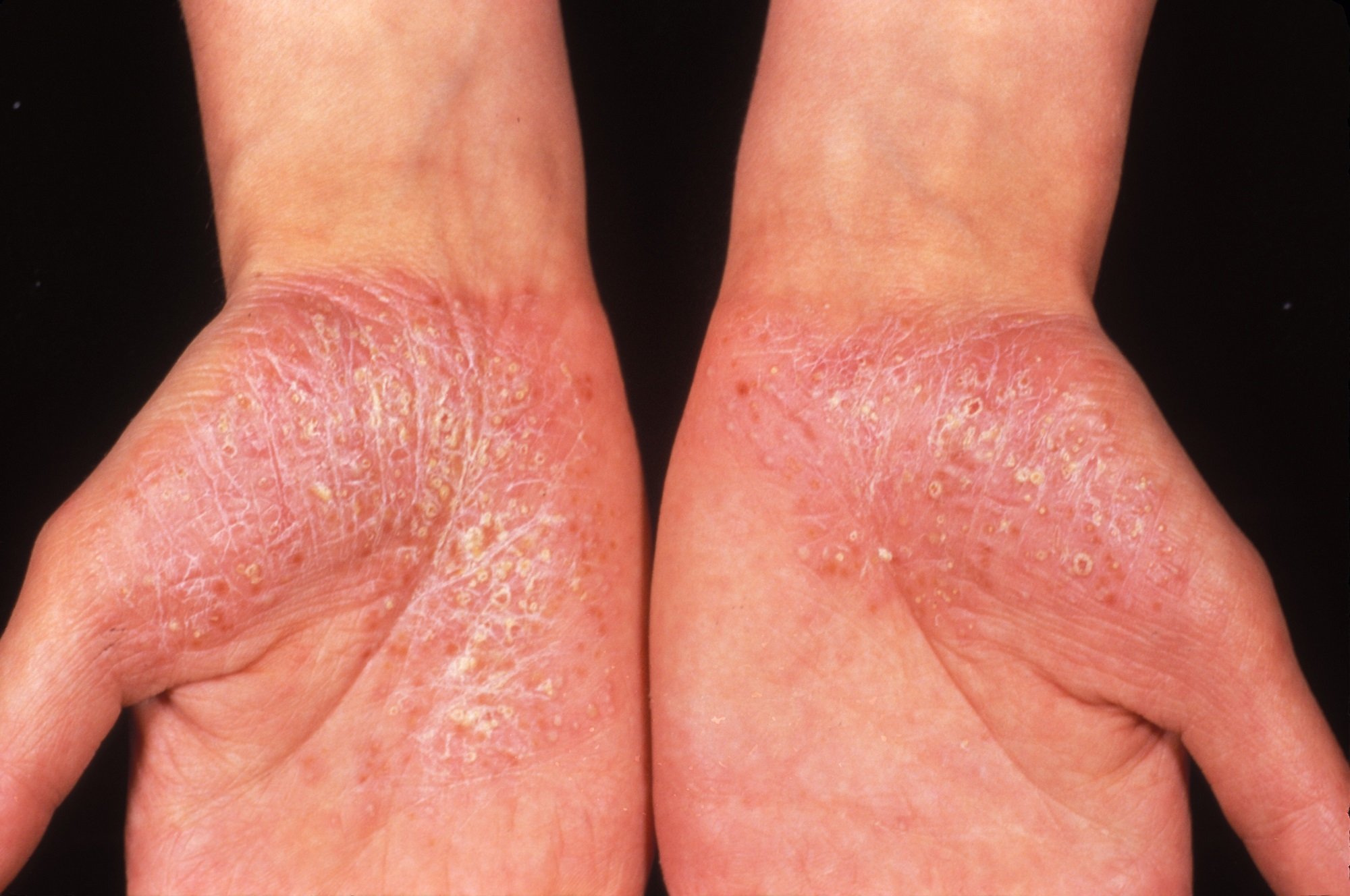
There are 2 main forms of localized pustular psoriasis: PPP and acrodermatitis continua . PPP is characterized by sterile pustules on the palmoplantar surfaces with yellow-brown macules. There may be scaly, erythematous plaques. A minority of patients has psoriatic plaques elsewhere, and the pustules primarily remain on the palmoplantar surfaces throughout the disease. PPP is thought to affect femalemore than male patients, with a ratio of approximately 3:1, and typically presents between the ages of 20 to 60. In contrast to plaque psoriasis, PPP is not associated with any HLA type. In epidemiologic surveys, PPP has been highly associated with smoking, and cessation of smoking is the most important measure to treat the disease.37 If a patient continues to smoke, PPP is highly resistant to treatment.
Acrodermatitis continua is a rare eruption of sterile pustules on the fingers or toes that slowly extends proximally. Chronic disease leads to atrophy of the digit and destruction of the nail matrix. It is difficult to treat.
Auli Toivanen, in, 2007
Read Also: Over The Counter Medicine For Plaque Psoriasis
Palmoplantar Pustulosis Or Psoriasis
Last week, I was presenting online about psoriasis. Whilst I was discussing variants of the condition, I mentioned pustular psoriasis particularly the type that exclusively affects the palms and soles of the feet which is known as palmoplantar pustulosis . For many years it has been considered to be a sub-type of psoriasis but recent literature has begun to challenge this theory suggesting PPP may be a separate disease. This article examines some of the evidence and looks at recent advances in its treatment.
PPP is characterised by erythema of the plantar surface which gradually becomes studded with sterile pustules of about 2-4mm diameter. These can coalesce to form larger lesions. Eventually, as they resolve they darken, dry out and eventually desquamate. The epidermis beneath them is fragile, erythemic and the condition is frequently accompanied by hyperkeratosis. Most patients describe how the condition relapses and remits just like psoriasis. Interestingly, research has also shown how frequently the two conditions may co-exist .
Other differences between PPP and psoriasis have been reported:
· PPP does not appear to share similar genetic susceptibilities with psoriasis.
· Psoriatic arthritis does not appear to be associated with PPP.
· Fewer nail abnormalities in patients with PPP than psoriasis
· Traditional treatments for psoriasis rarely improve PPP
Treatment
Please read another article which I published on this subject – available here
References
This Site Does Not Provide Medical Advice:

The content provided on this website is for educational and informational purposes only, and is not intended as a substitute for advice from a qualified medical professional. The views and opinions expressed on this website are those of the authors, and are not intended to serve as diagnosis, treatment, or prevention of disease. Always consult with your doctor regarding your medical condition or any symptoms you may be experiencing.
Sign up for periodic emails with resources, insights, and updates on autoimmune disease and living with chronic illness.
You May Like: Is Red Light Therapy Good For Psoriasis
> > > Best Psoriasis Cure Available
3. To help safeguard the skin, the immune system release chemicals that can cause nerves to itch and blood vessels to dilate to prepare the skin for a sudden rush of immune cells
4. When the immune cells arrive at the scene, most work to kill off the pathogens causing the distress, but a few capture some of the invaders and take them back to the heart of the immune system, where other soldier cells are produced in a way to recognize and attack the invading cells on contact
5. Inflammation is the bodys way of opening blood vessels to allow more soldier cells to rush to the battlefield.
While this entire process is completely normal, people with psoriasis tend to overproduce these soldier cells when the body feels threatened. This overabundance of killer immune cells can actually be dangerous to the skin since they begin to attack good cells along with the bad ones.
While it is great to finally understand the impact an improperly working immune system can have on your skin and cause psoriasis more research is needed to pinpoint the exact cause for the over-firing of the cell messages. Palmoplantar Pustular Psoriasis Vs Palmoplantar Pustulosis
What Is The Treatment Of Palmoplantar Pustulosis
Treatment of palmoplantar pustulosis does not cure the disorder and is not always successful. The following may be helpful.
General Measures
- If you smoke, try to stop: however, palmoplantar pustulosis may take several months or longer to improve.
- If you have coeliac disease, follow a strict gluten-free diet.
- If you have recurrent tonsillitis, consult an otolaryngologist to see if a tonsillectomy is recommended.
- Choose comfortable footwear made from natural fibres.
- Avoid friction and minor injuries.
- Cover deep fissures with a waterproof dressing.
- Rest the affected area.
- Use plenty of a thick emollient to soften the dry skin to prevent fissures.
- Soak in warm water with emulsifying ointment for 10 minutes.
- Apply soft white paraffin liberally
- Use salicylic acid ointment, ureacream or a heel balm to peel off dead skin .
- Wash using bath oil or soap substitute.
Topical steroidsTopical steroids are anti-inflammatory agents which range in potency and vehicle. Only the strongest ointments are effective in conditions affecting the thick skin of the hands and feet. However, the very potent products such as clobetasol propionate should be used only for limited periods or else side effects and loss of efficacy become a problem.
A thin smear should be applied twice daily to the affected area. The effect may be enhanced by using plastic occlusion for a few hours or even overnight use polythene gloves, plastic bags or cling film. Do not use occlusion for more than five days in a row.
Also Check: Hydrocortisone Cream For Scalp Psoriasis
Palmoplantar Psoriasis: A Review Of Topical Therapies
Linden Li
Department of Dermatology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Peter W Hashim
Department of Dermatology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Grace Kimmel
Department of Dermatology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
John K Nia
Department of Dermatology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
DOI: 10.15761/GOD.1000196
Extraarticular Features And Imaging
The seronegative spondyloarthropathies are associated with a wide spectrum of extraarticular clinical manifestations, although imaging plays a relatively small role in the diagnosis of these features. Organ systems that may be involved include the skin, gastrointestinal tract, eye, heart, lung, kidney, and GI tract.119
Ankylosing Spondylitis
An association between AS and IBD is well documented, and the presence of occult mucosal inflammation in the bowel of patients with AS has been detected in more than 50% of AS patients.120
The most common extraarticular feature of AS is acute anterior uveitis, which may be the presenting symptom.121 At presentation, the involvement is usually unilateral with the inflammation subsiding in a few weeks, but there is a tendency for recurrence, often in the contralateral eye.
Cardiac involvement is not uncommon and most frequently consists of aortic root inflammation that can lead to aortic incompetence.122 Extension of the inflammation into the conduction system may result in partial or complete heart block.
Apical pulmonary fibrosis with bullous changes has been reported as an uncommon and usually late complication of AS , but high-resolution CT suggests that this process may be underrecognized with conventional radiography.123
Apical pulmonary fibrosis may be a late complication of AS.
Reactive Arthritis and Spondyloarthropathy
Pulmonary and renal involvement are not prominent features of reactive arthritis.
Psoriatic Spondyloarthropathy
You May Like: How To Get Rid Of Psoriasis In Hair
Risk Factors For Pustular Psoriasis
The following factors can reportedly trigger an eruption of pustular psoriasis:
- Withdrawal of systemic steroids, potent topical steroids, or cyclosporine
- Drugs, including salicylates, iodine, lithium, phenylbutazone, oxyphenbutazone, trazodone, penicillin, hydroxychloroquine, calcipotriol, interferon-alpha, recombinant interferon-beta injection, terbinafine, and bCG vaccination
- Strong, irritating topical medications, including tar, anthralin, steroids under occlusion, and zinc pyrithione in shampoo
- Cutaneous infections
- Sunlight or phototherapy
Update On Diagnosis Treatment Options For Palmoplantar Pustulosis
An overview of the current methods involved in diagnosis, screening, and treatment of palmoplantar pustulosis was provided in a review published in Clinical, Cosmetic and Investigational Dermatology.
The disease, which may manifest as sterile, erupting pustules located on the soles of the feet and palms of the hands also presents with nail changes in more than 40% of patients. Irritant contact dermatitis, dyshidrotic eczema, pityriasis rubra pilaris, pompholyx, fungal infections, and acrodermatitis comprise the differential diagnosis of PPP. Triggering factors of PPP include smoking, infections , psychological stress, allergies, and some drugs .
The standard treatment approach to PPP, although challenging, typically involves the use of topical and systemic therapies in addition to phototherapy and targeted molecules. There exists no gold standard in terms of therapy, and no available treatment is considered curative for the disease. Currently, control of mild PPP may be achieved with the use of on-demand occlusion of topical therapies. Arguably the best treatment option in this sense is oral acitretin, a vitamin A derivative, in combination with psoralenultraviolet A .
Disclosure: Several study authors declared affiliations with the pharmaceutical industry. Please see the original reference for a full list of authors disclosures.
Reference
Don’t Miss: What To Eat If You Have Psoriasis