Swollen Fingers Or Toes
PsA may begin in smaller joints, such as those of the fingers or toes, and progress from there.
Spondylitis may be accompanied by dactylitis, or swelling of the toe or finger joints. This is sometimes called sausage fingers.
Dactylitis is estimated to affect up to 50 percent of patients with PsA, and is uncommon in other types of arthritis, except gout or pseudogout.
When caused by PsA, dactylitis may affect individual digits differently. For example, your left hand may be swollen while your right is not.
Unlike other types of arthritis, PsA tends to make your entire finger or toe appear swollen, rather than just the joint.
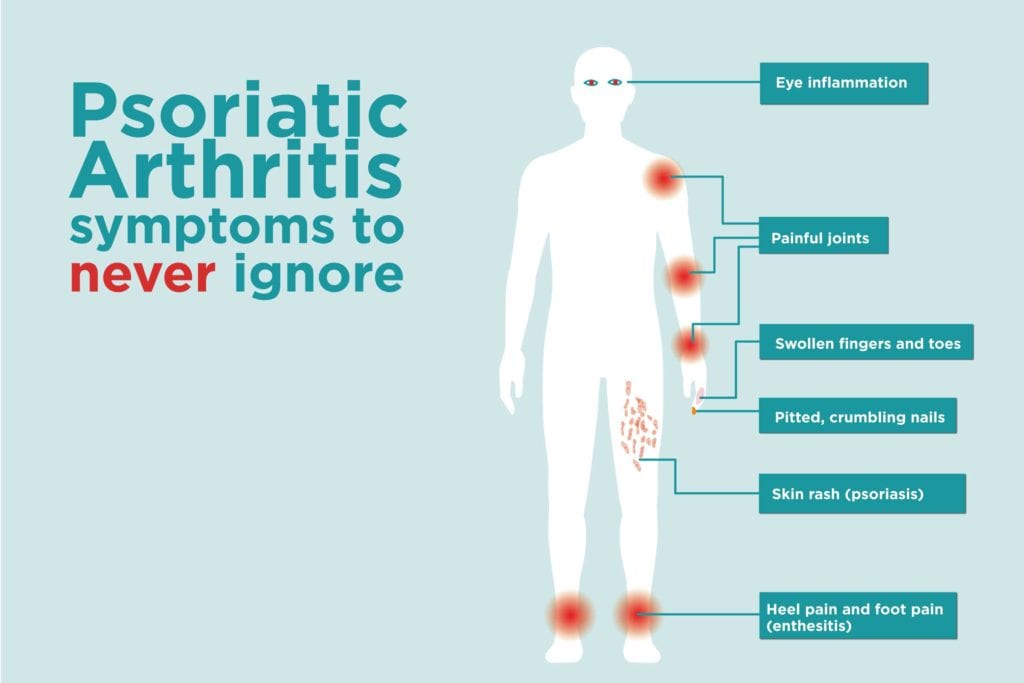
People with PsA may experience eye problems, such as inflammation and redness. Symptoms of eye inflammation include:
- red eyes
- dry eyes or feeling of grit or sand in the eyes
- difficulty focusing or blurred vision
- pain or sensitivity, especially to bright light
- floaters, or small specks, lines, or other shapes in your field of vision
If you develop new or large floaters along with flashing lights in your field of vision, it may be a sign of a medical emergency. Seek immediate treatment from a qualified medical professional.
You may also experience uveitis, or inflammation of the middle layer of the eye called the uvea. Between 7 and 25 percent of people with PsA develop uveitis.
Symptoms of uveitis include:
How Does It Affect Cartilage
In arthritis, the cartilage at the end of the bones becomes damaged and breaks down. In PsA, this damage results from persistent inflammation. As the cartilage erodes, the bones rub together, causing further pain and joint damage. Inflammation can also lead to bone erosion and extra bone growth.
Chronic inflammation can also affect the ligaments and tendons around the joint.
What Will Happen To Me
With the right treatment, most people with psoriatic arthritis can lead full and active lives. However the course of psoriatic arthritis is variable and no two cases are the same. Many people find their symptoms worsen at times and then settle down for a period of time. About one in 20 people with psoriatic arthritis will develop a more severe, destructive form which can cause deformity to the joints in the hands and/or feet. Most people with psoriatic arthritis will need some ongoing treatment to control their symptoms and prevent damage to the joints. This is usually managed by a rheumatologist.
Don’t Miss: How Does One Develop Psoriasis
Youre Having Problems With Your Eyes
The inflammation from psoriatic arthritis can even target your eyes, says Ludmer. In fact, some research says between 7% and 20% of people with psoriatic arthritis appear to develop uveitis, a serious form of inflammation in the tissue of the eye wall that can lead to irreversible vision loss, according to the Mayo Clinic. Early warning signs of this condition include pain and redness in the eyes, light sensitivity, blurred vision, and floaters in your field of vision.
You Feel Pain In Your Heel Every Time You Take A Step
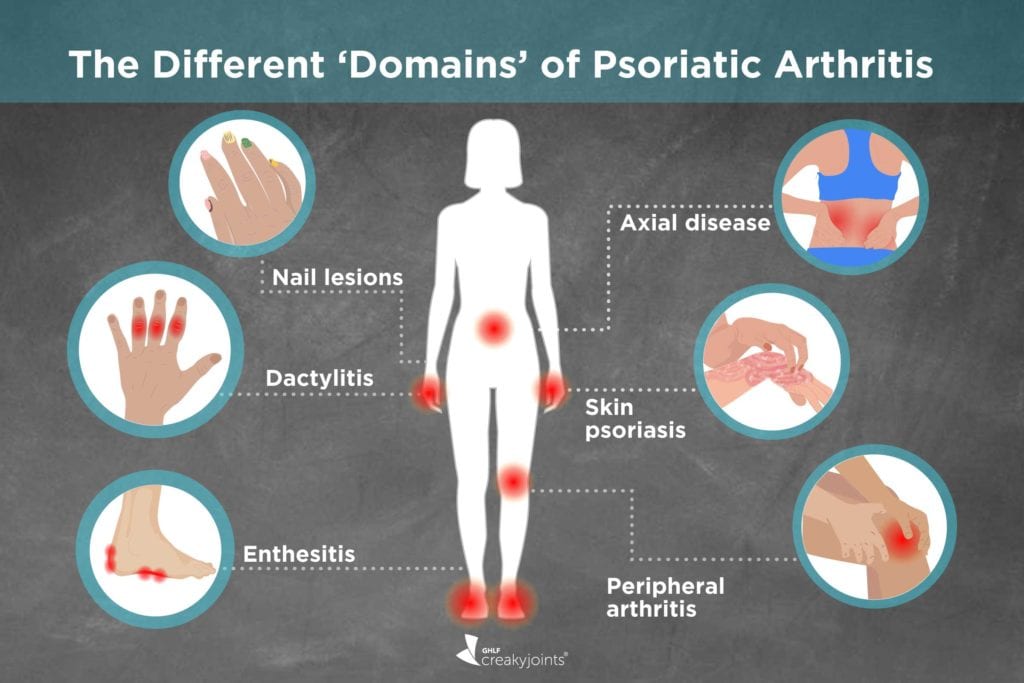
Psoriatic arthritis also has a tendency to cause inflammation in sites where tendons insert into bones, such as the Achilles tendon at the back of the heel, and the plantar fascia, causing pain in the sole of the foot and bottom of the heel which often will interfere with walking, says Dr. Rosenstein.
While experts say this isnt the most common psoriatic arthritis symptom, it can make life with this condition even more difficult. If you have heel pain that you cant explain with other reasons , you should get it checked out by a doctor.
Recommended Reading: Psoriasis Treatment Creams Over The Counter
Classification Of Psoriatic Arthritis
The simple and highly specific Classification Criteria for Psoriatic Arthritis , developed by a large international study group, has a sensitivity and specificity of 98.7% and 91.4%, respectively. The criteria consist of established inflammatory articular disease with at least 3 points from the following features:
- Current psoriasis
- A history of psoriasis
- A family history of psoriasis
- Dactylitis
- Juxta-articular new-bone formation
- RF negativity
- Nail dystrophy
Does Diet Make A Difference
- No particular diet is uniformly effective some people with psoriatic arthritis have found cutting down on saturated fats helps and may reduce the doses needed of other treatments, though research has not confirmed this.
- Dietary supplements such as evening primrose oil and certain fish oils may have a variable effect. They are safe and have other health benefits, but effects specifically beneficial to psoriatic arthritis have not been proven in research.
- Following guidelines about healthy lifestyle, keeping weight down and moderating alcohol intake are all generally accepted as beneficial regardless of having psoriasis or psoriatic arthritis. Keeping weight in the healthy range has been shown to improve the likelihood of responding to medication. See Psoriatic Lifestyle
Remember: many so-called cures for arthritis are not proven by clinical trials to be of use and may be driven by profit to those advocating them.
Don’t Miss: Do African Americans Get Psoriasis
Fatigue: A Common Problem That Can Worsen Pain
People who have psoriatic arthritis report higher levels of fatigue than those without the condition, according to a study published in January 2020 in the journal Dermatology. Psoriatic arthritis is a systemic inflammatory condition, Gupta says. Left untreated, it can result in fatigue and a general feeling of sickness. It can also result in anemia due to prolonged inflammation.
Unchecked fatigue can worsen your pain and vice versa, so talk to your doctor about adding pain management and sleep strategies to your psoriatic arthritis management plan.
Risk Factors For Inflammation
Risk factors for the inflammation that leads to psoriatic diseases arent fully understood. One study showed an almost 50-times greater chance of developing psoriatic arthritis if you have a close family member who has had the condition. Genetics appear to play a role, but its unclear if family history alone is a good predictor of whether or not someone will develop PsA.
Other risk factors for the development of psoriatic arthritis may include age, environment, smoking, and obesity.
- Age For most people, psoriatic arthritis begins between ages 30 and 50. It usually begins five to 10 years after the first diagnosis of psoriasis.
- Environmental factors Stress, chronic illness, and some infections may contribute to the development of psoriatic arthritis.
- Smoking The more heavily a person smokes, the greater their risk of developing psoriatic arthritis. People who have smoked in the past are more likely to develop PsA than those who have never smoked.
- Obesity People who have psoriasis and obesity are more likely to develop psoriatic arthritis.
Its important to note that stress, chronic illness, smoking, and obesity worsen inflammation in the body in a general sense. Obesity and smoking trigger the release of inflammatory chemicals on their own. When combined with another source of inflammation, they may compound.
| How do skin and joint pain affect your life?Have you found ways to manage the symptoms?Click in the comments below. |
Don’t Miss: Psoriasis Fotos En Las Manos
You Have Pain Or Burning In Your Elbow
A condition called tennis elbow can sometimes show up as a symptom of psoriatic arthritis, even if youve never picked up a racquet. Again, this has to do with the inflammation that happens in spots where your tendons connect to bones, says Dr. Rosenstein. You might notice pain or burning in the external part of your elbow, along with poor grip strength, per the American Academy of Orthopedic Surgeons.
Do We Know What Causes Psoriatic Arthritis
- The cause of psoriatic arthritis is the subject of much research.
- You cannot catch psoriatic arthritis or psoriasis from someone else. Therefore they are not contagious.
- The cause of psoriatic arthritis is not proven but experts believe it to be a combination of genetic, immunological and environmental factors. 2 out of 5 people with psoriasis or psoriatic arthritis have a first-degree relative with the condition. This means you have a higher chance of developing psoriasis or psoriatic arthritis if you have relative who has the condition. Some experts believe infections such as streptococcal infections may provoke psoriatic arthritis, though this is not proven.
- The role of bacteria in the gut and developing psoriatic arthritis is the subject of current research.
- Trauma and stress may be contributing factors, although this is not proven.
- The genetic make-up of an individual is likely to determine the risk of developing psoriasis and psoriatic arthritis and probably influences the severity.
- Being overweight is now understood to be linked to developing psoriatic arthritis and is the subject of ongoing research.
- There are certain genetic markers linked to the immune system which are now being used to predict the severity of psoriatic arthritis. Much more is known about the mechanisms that lead to inflammation in other conditions and it is likely advances in science will lead to much more effective treatments with fewer side effects.
Don’t Miss: Get Rid Of Psoriasis Fast
What Causes Psoriatic Arthritis
The cause of psoriatic arthritis is unknown. Researchers suspect that it develops from a combination of genetic and environmental factors. They also think that immune system problems, infection, obesity, and physical trauma play a role in determining who will develop the disease. Psoriasis itself is neither infectious nor contagious.
Recent research has shown that people with psoriatic arthritis have an increased level of tumor necrosis factor in their joints and affected skin areas. These increased levels can overwhelm the immune system, making it unable to control the inflammation associated with psoriatic arthritis.
When Psoriatic Disease Strikes The Hands And Feet
We take many common movements and activities for granted â until they become difficult or impossible to do. Get a grip on whatâs happening.
Our hands and feet are ultra-sensitive. Sensory neurons, which trigger pain sensations in the brain, cluster at the fingertips. The complex anatomical structure of hands and feet â with many joints, tendons and ligaments packed tightly together â gives us an acute sense of touch and lets us do precision movements. Our hands, particularly when used for communication through gesture, draw attention.Our feet are so important for our balance and mobility.
Thatâs why psoriatic disease, when it strikes the hands and feet, has an outsize effect. The symptoms can be more intense and more upsetting. Fingernail psoriasis, for instance, is often immediately noticeable and can make something as basic as a handshake feel uncomfortable. Pain and other symptoms of psoriasis and psoriatic arthritis in the hands and feet can make other routine tasks hard to accomplish.
Gary Bixby, who lost all his fingernails and toenails to severe psoriasis , says psoriatic nail disease makes it painful to chop fuel for his wood-burning stove, a frustrating problem during winters at his home in Blair, Wisconsin.
âIt was affecting more fingernails, then my toenails and large areas on my arms, legs and trunk,â says Bixby. âThatâs when I went to a podiatrist, who thought I had psoriasis, and then to a dermatologist, who confirmed it.”
Also Check: Mejor Tratamiento Para La Psoriasis
Can Psoriatic Arthritis Affect Other Parts Of The Body
Having psoriatic arthritis can put you at risk of developing other conditions and complications around the body.
The chances of getting one of these are rare. But its worth knowing about them and talking to your doctor if you have any concerns.
Eyes
Seek urgent medical attention if one or both of your eyes are red and painful, particularly if you have a change in your vision. You could go to your GP, an eye hospital, or your local A& E department.
These symptoms could be caused by a condition called uveitis, which is also known as iritis. It involves inflammation at the front of the eye.
This can permanently damage your eyesight if left untreated.
Other symptoms are:
- blurred or cloudy vision
- sensitivity to light
- not being able to see things at the side of your field of vision known as a loss of peripheral vision
- small shapes moving across your field of vision.
These symptoms can come on suddenly, or gradually over a few days. It can affect one or both eyes. It can be treated effectively with steroids.
Heart
Psoriatic arthritis can put you at a slightly higher risk of having a heart condition. You can reduce your risk by:
- not smoking
- staying at a healthy weight
- exercising regularly
- eating a healthy diet, thats low in fat, sugar and salt
- not drinking too much alcohol.
These positive lifestyle choices can help to improve your arthritis and skin symptoms.
Talk to your doctor if you have any concerns about your heart health.
Crohns disease
Non-alcoholic fatty liver disease
Depression: A Sadness You Cant Shake
People who have psoriatic arthritis often struggle with emotional distress theyre not prepared to deal with, according to a review published in January 2020 in the journal Acta Dermato-Venereologica.
Persistent sadness or hopelessness, withdrawing from your circle of friends, and loss of interest in activities you once enjoyed are potential symptoms of depression. Signs of depression are common in people who have psoriatic arthritis due to social withdrawal due to skin lesions and the inability to do the tasks they were previously able to do, Gupta says.
The severity of your psoriatic arthritis isnt necessarily related to your risk of developing depression or another mental health issue, he says, but if your psoriatic arthritis is well controlled, it may help with depression.
If youre experiencing symptoms of depression, be sure to talk to your doctor.
Recommended Reading: Psoriasis Treatment Center Of Central New Jersey
Tlc For Hands And Feet
Avoiding injuries, even small ones , makes good sense for people with psoriasis or PsA affecting the hands and feet.
âThe Koebner phenomenon is the flaring of psoriasis in response to injury. Even minor trauma can cause a flare,â says Duffin. âFor example, if you use your nails to pry open a lid, youâre probably going to make your nail psoriasis worse.â
Similarly, shoving feet into shoes without enough room to wiggle toes or wearing high heels means youâre putting constant pressure on nails and joints, which can increase pain and nail problems.
âI generally recommend flats that have good cushioning and arch support that takes the weight off toe joints â which doesnât mean wearing ballet slippers that have no padding in the bottom,â says Gottlieb.
âYou donât want a triangle profile that squeezes the toes, because that elicits pain.â She also cautions that flip-flops, a summer favorite, expose toes and feet to trauma.
A consultation with a podiatrist, who can advise on the right footwear and design an orthotic for individual foot issues, is often helpful for people with PsA that affects the feet, Gottlieb says.
Treatment For Muscle And Joint Pain
In case you dont have any other symptoms that would indicate having one of the conditions described below consider using some homemade treatments to ease the pain.
Here is what you can do to relieve muscle discomfort:
Read Also: What Are Biologic Drugs For Psoriasis
Getting A Diagnosis Of Psoriatic Arthritis
The presence of psoriasis may provide an indication of psoriatic arthritis when someone develops joint symptoms. Psoriatic arthritis can develop in people with a lot or a little of psoriasis, and may be more common in people with nail psoriasis. As well as joint symptoms, psoriatic arthritis can lead to feeling tired. Many people become frustrated by a lack of diagnosis psoriatic arthritis tends to have periods of improvement and worsening, which may also be attributed to mechanical joint problems and not inflammatory arthritis.
If you have the symptoms of inflammatory arthritis, such as psoriatic arthritis, your doctor will often refer you to a rheumatologist. In some cases, further tests and imagery may be sought, although this will depend on the individual circumstances and level of confidence in the initial diagnosis.
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
Also Check: What Is The Life Expectancy Of Someone With Psoriasis
Diagnosing And Treating Psoriatic Arthritis
Having a physical exam is the first step to diagnosing and treating PsA. Your physician will talk with you about ongoing symptoms. Let your physician know if you have a family history of PsA, psoriasis or other autoimmune diseases. Your health care provider will also check for tenderness, swelling, limited movement, and skin or nail changes.
Read More: Aging With Arthritis
There is no cure for PsA. But that doesn’t mean you cant manage the disease and have a healthy, active life. You can work with your health care team to find the best treatment for you.
Treatment varies based on how the disease affects your life, Dr. Jones says. If you have mild symptoms, you may only need treatment during flare-ups. People with severe psoriatic arthritis may need a more aggressive treatment plan to reduce inflammation and improve quality of life.
Medications For Pain Relief

If your muscle pain is negatively affecting your quality of life or causing you significant discomfort, medications may help relieve it. Over-the-counter non-steroidal anti-inflammatory drugs like ibuprofen or naproxen could help. However, if you are already taking NSAIDs for psoriatic arthritis, you should consult your rheumatologist before taking more.
You may also ask your doctor about muscle relaxants. Although muscle relaxants have not been shown to help with psoriatic arthritis itself, they could help reduce your muscle pain especially if it is extreme.
Read Also: What Does Scalp Psoriasis Feel Like