What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
Reviewpsoriasis As An Autoimmune Disease Caused By Molecular Mimicry
Psoriasis is strongly associated with streptococcal throat infection, and patients have increased occurrence of such infections. Psoriatic lesional T cells are oligoclonal, and T cells recognizing determinants common to streptococcal M-protein and keratin have been detected in patients blood. We propose that CD8+ T cells in psoriatic epidermis respond mainly to such determinants, whereas CD4+ T cells in the dermis preferentially recognize determinants on the streptococcal peptidoglycan that might itself act as an adjuvant. The streptococcal association might reflect the concurrence of superantigen production promoting skin-homing of tonsil T cells, M-protein mimicking keratin determinants, and adjuvant effects of the peptidoglycan. Accordingly, improvement of psoriasis after tonsillectomy should be associated with fewer T cells that recognize keratin and streptococcal determinants.
- Previous article in issue
Treating Psoriatic Disease Is Key
Untreated inflammation is dangerous, stresses Dr. Mehta.
âYou need to treat psoriasis no matter what its severity,â he says. âIf youâre ignoring it, your body is doing things on the inside that you donât know about until later. People who donât treat severe disease, for example, are growing coronary plaque at an alarmingly fast rate.â
Those with mild disease also need treatment, says Dr. Mehta. âItâs my personal opinion, and not yet part of the guidelines, but I think even one psoriatic plaque is too much,â he says.
Thereâs evidence that treatment with biologics reduces incidences of heart disease and heart attacks, says Dr. Mehta. He, Dr. Yamauchi and Dr. Ogdie say they also suspect treatments that control systemic inflammation may lower the risk of other comorbidities of psoriasis, including PsA.
âWe think itâs probably true that if you treat your psoriasis, youâre more likely to prevent psoriatic arthritis, delay its onset or reduce its severity if it does develop,â Dr. Ogdie says. âBut we still donât yet have the data to say that definitively.â
Read Also: Are Baths Good For Psoriasis
Why Psoriasis Is An Autoimmune Condition
Casey Gallagher, MD, is board-certified in dermatology. He is a clinical professor at the University of Colorado in Denver, and co-founder and practicing dermatologist at the Boulder Valley Center for Dermatology in Colorado.
Psoriasis causes a variety of symptoms that range from merely irritating to actually debilitating. The symptoms can include thick, red patches on the skin pitted, ridged fingernails scaly, itchy scalp and hair loss and stiff, painful joints.
Why do some people, but not others, get this frustrating condition in the first place? Arriving at an answer to this question relies partly on knowing that psoriasis is an autoimmune disorder “auto” meaning self and “immune” referring to the body’s complex immune system.
What Are The Types Of Psoriasis
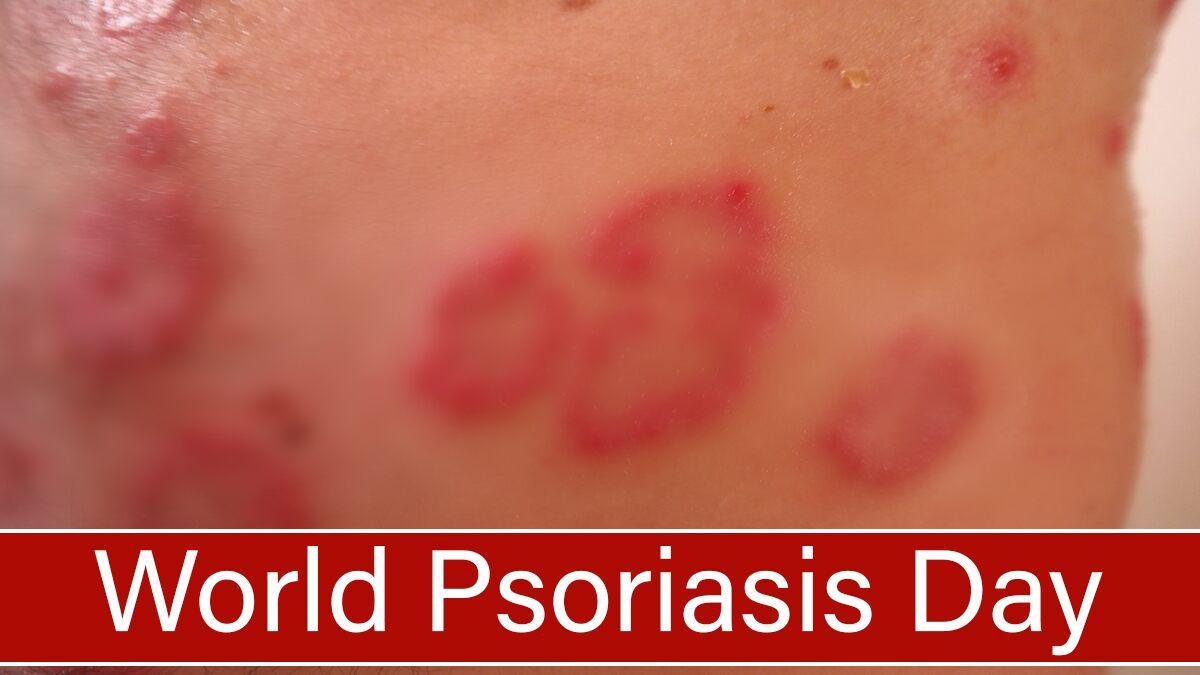
There are different types of psoriasis, but the most common kind isplaque psoriasis. It appears as raised, red patches of skin that are covered by silvery-white scales. The patches usually develop in the same pattern on both sides of the body and tend to appear on the:
- Scalp.
- Limbs, especially the elbows and knees.
Also Check: Best Way To Cure Psoriasis
Treatments That Target The Immune System
Treatment for psoriasis depends on the type and severity of the condition, your general health, and other factors.
Here are the various treatments that target specific factors in the immune system that cause inflammation. These are generally used when your psoriasis symptoms are moderate to severe. Note that the newer drugs are more expensive.
Psoriatic Disease Affects More Than Skin And Joints
The systemic inflammation that drives symptoms of psoriatic disease can raise your risk for other health problems.
If you have psoriasis or psoriatic arthritis , you may know that these diseases raise your risk for some other conditions as well. When one disease is triggered by or linked to another, the related condition is called a âcomorbidity.â PsA, for example, is a common comorbidity of psoriasis, affecting up to 33 percent of people with psoriasis.
According to the recent Joint AAD-NPF Guidelines of Care for the Management and Treatment of Psoriasis with Awareness and Attention to Comorbidities, other comorbidities for which psoriatic disease raises risk include:
- Cardiovascular disease
- Mental health impacts, including depression and anxiety
- Inflammatory bowel disease
- Uveitis
- Nonalcoholic fatty liver disease
Just how this elevated risk happens for each comorbidity isnât fully understood. One underlying factor that likely plays an important role in triggering or contributing to development of many comorbidities, however, is systemic inflammation, explains dermatologist Paul S. Yamauchi, M.D., Ph.D.
The weapons the immune system uses for this attack are inflammatory immune cells that normally defend the body from injury and infection.
Also Check: Can Psoriasis Be On The Face
How Does Psoriasis Weaken Your Immune System
Psoriasis develops when your immune system is overactive.
Your body produces an excess of inflammatory agents called cytokines, which normally help the body fight infections and heal injuries. But instead of fighting off unhealthy cells, these cytokines attack healthy cells. Your white blood cells are kept in a hyperactive state and your body in a pro-inflammatory condition, making you more susceptible to common colds and flu.
Additionally, the steroids used to control your flares directly can weaken your immunity by reducing white cell function.
What Happens During Psoriasis Autoimmune Attacks
In people with psoriasis, the immune system attacks autoantigens on tissues in the skin. These autoantigens include protein products made by the skin cells. Studies have identified the presence of these autoantigens in psoriatic lesions.
Autoantigens are believed to activate T cells and other cells of the immune system. T cells can destroy tissue and produce inflammatory chemicals such as interleukin-17A that promote the abnormal growth of skin cells.
Other immune cells, known as B cells, can also contribute to autoimmunity in psoriasis. B cells produce proteins known as antibodies that can help destroy antigens. In people with psoriasis and psoriatic arthritis , B cells make antibodies against the autoantigens associated with the skin. Antibodies made against autoantigens are referred to as autoantibodies.
Ultimately, the dysfunction and autoimmune activity of the immune system in psoriasis leads to the severe inflammation that contributes to overactive skin cell growth and psoriatic lesions or joint damage. High levels of inflammation from the overactive immune system may also be behind a higher risk for heart disease in people with psoriasis.
Also Check: Is Vicks Vaporub Good For Psoriasis
Systemic Autoimmune Rheumatic Diseases And Coinciding Psoriasis: Data From A Large Single
Anna Bazsó
1National Institute of Rheumatology and Physiotherapy, Frankel Leó Utca 38-40, Budapest 1023, Hungary
2Institute of Immunology, Rikshospitalet, Oslo University Hospital, 0027 Oslo, Norway
Abstract
Psoriasis is a systemic immune-inflammatory disease characterized by chronic or recurrent skin symptoms, psoriatic arthritis, enthesopathy, and uveitis. Psoriasis has recently been published to appear with various autoimmune disorders, but the coexistence has been systematically reviewed by only few studies until now. In the present study, charts and electronic database of 4344 patients with various systemic autoimmune disorders, under regular medical control at our department, were reviewed retrospectively searching for association with psoriasis. Hereby, we demonstrate 25 psoriatic patients coinciding with various systemic autoimmune diseases. The coexistence of psoriasis and autoimmune diseases resulted in the worsening of the clinical outcome of the autoimmune diseases as indicated by higher frequency and dosages of glucocorticoid use, need for biologicals, and other comorbidities. These results suggest common environmental and genetic background as well as therapeutic possibilities in the future.
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Summary
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Obesity Metabolic Syndrome And Diabetes
Obesity is the most common comorbid condition in people with both psoriasis and PsA, says Dr. Ogdie. It sets the stage for insulin resistance and type 2 diabetes.
Insulin resistance means the body is less able to move glucose, a type of sugar your body uses for energy, from the blood into cells. Glucose builds up in the blood and begins the processes that cause type 2 diabetes, another risk factor for heart disease and stroke.
âIn addition, in people with psoriatic disease, obesity is linked to not responding well to treatment and to worse quality of life and function,â Dr. Ogdie says. âIn people with psoriasis, itâs the single greatest risk factor for development of psoriatic arthritis. For those with psoriatic arthritis, obesity creates an extra burden for joints already affected by disease.â
The relationship among inflammation, obesity and related comorbid conditions is complicated, says Dr. Mehta.
âWe think inflammation from the overactive immune system is getting into the adipose, or fat, tissue,â he says. âOur bodies have insulin receptors on adipose tissue, and when you have more fat, youâre more likely to become insulin resistant â and thatâs prediabetes.â
Also Check: Is Humira Used For Psoriasis
Environmental Triggers Of Psoriasis
Several environmental factors including physical trauma, drug reactivity, infection as well as modifiable variables such as psychological stress, obesity, smoking, and alcohol have been associated with a predisposition toward psoriasis development and exacerbation of the disease.
Physical trauma
Heinrich Koebner first described physical trauma as a trigger and exacerbating factor for psoriasis in 1872. He observed the development of psoriatic lesions after a direct cutaneous injury, such as excoriation, tattoos, burns, and animal or insect bites, in previously normal-appearing skin . The new psoriatic lesion was characterized morphologically as identical to the injury site, known as an isomorphic response. The Koebner response has been observed with other dermal diseases such as vitiligo and lichen planus, but the frequency for its manifestation is higher among psoriasis patients. The prevalence of Koebner response in psoriasis patients ranges from 24%51%.
Psoriasis onset following an injury may take anywhere from 3 days to 2 years to develop, and may be dependent on seasonal variation as well as disease severity .,
Drug-induced psoriasis
Other reported medications that exacerbate psoriasis include ACE inhibitors, calcium channel blockers, and IL-2 among others.
Infections
Stress
Alcohol and smoking
Obesity
The Bodys Defenses Gone Rogue

Researcher Nehal N. Mehta, M.D., MSCE, is a senior investigator in the Section of Inflammation and Cardiometabolic Diseases at the National Heart, Lung, and Blood Institute in Bethesda, Maryland. For the past six years, he and other scientists in his NHLBI lab have followed a group of 350 people with plaque psoriasis, looking into how chronic inflammation affects their risk of heart disease and metabolic conditions such as diabetes.
âInflammation is simply a collection of immune cells trying to put out a fire, and that fire is usually an infection or some sort of virus,â says Dr. Mehta, a cardiologist and internist.
Setting off this inflammatory response, infiltration of immune cells and release of factors, is what the immune system evolved to do. In psoriatic disease, however, this primal defense has gone awry.
âIn psoriasis, immune cells attack places they shouldnât,â Dr. Mehta says. âThey go to the skin and cause psoriatic plaques, but they can also go to the joints and cause psoriatic arthritis. When they infiltrate blood vessels of the heart, they inflame the cells that line blood vessels. These fill with immune cells that donât belong there and cause inflammation. Thatâs the beginning of cardiovascular disease.â
You May Like: Does Zinc Help With Psoriasis
Psoriasis And The Immune System
disagree . One alternative theory is that psoriasis occurs because the immune system reacts irregularly to bacteria on the skin due to genetics.
In an autoimmune disease, specific triggers cause the immune system to malfunction. These triggers vary between individuals. But in the case of psoriasis, they can include stress and skin trauma, such as insect bites, sunburn, and scratches.
In psoriasis, the activated immune system mistakenly launches an inflammatory response. It begins to attack healthy cells as though they were harmful invading pathogens. White blood cells called T helper lymphocytes, or T cells, become irregularly active and produce excess signaling molecules.
These cytokine molecules cause the blood vessels in the skin to widen. In turn, this causes white blood cells to accumulate, and keratinocytes, which make up the outer layer of the skin, to multiply much faster than usual.
In psoriasis, the process of a cell dividing, maturing, migrating to the skins surface, and sloughing off is complete in as few as 37 days, compared with 34 weeks in a person without psoriasis.
The result of this skin buildup is thickened, flushed, and scaly skin plaques.
| extra-virgin olive oil |
How Is Psoriasis Diagnosed And Treated
Psoriasis often has a typical appearance that a primary care doctor can recognize, but it can be confused with other skin diseases , so a dermatologist is often the best doctor to diagnose it. The treatment of psoriasis usually depends on how much skin is affected, how bad the disease is , or the location . Treatments range from creams and ointments applied to the affected areas to ultraviolet light therapy to drugs . Many people who have psoriasis also have serious health conditions such as diabetes, heart disease, and depression. Some people with psoriasis also have an inflammatory condition which affects their joints, called psoriatic arthritis.
Psoriatic arthritis has many of the same symptoms as other types of arthritis, so a rheumatologist is often the best doctor to diagnose it. The treatment of psoriatic arthritis usually involves the use of drugs .
Psoriatic disease may be treated with drugs or a combination of drugs and creams or ointments.
You May Like: How Can Psoriasis Be Treated
Foods To Eat If You Have Psoriasis
Just as some foods trigger inflammation, others can help combat inflammation. In general, having a balanced whole-foods diet is the best approach to reduce inflammation throughout the body. It may reduce psoriasis flare-ups or make your symptoms less severe. Following a Mediterranean diet for psoriatic arthritis or psoriasis can also reduce chronic inflammation that contributes to heart disease, type 2 diabetes, cancer and other conditions.
The best foods if you have psoriasis include:
- Fish, lean protein or plant-based proteins such as tofu or tempeh
- Fruits and vegetables
- Small amounts of low-fat dairy
- Whole grains
Theres no evidence that vitamins or supplements help ease psoriasis symptoms. The best way to get all the vitamins and minerals you need is from the foods you eat. But its generally safe to take a daily multivitamin. Talk to your doctor or a registered dietitian about other supplements that might be right for your needs.
What Is An Autoimmune Disorder
Your body’s immune system is responsible for fighting foreign invaders threatening your health: bacteria, viruses, and fungi are just a few examples. Your good health depends partly on two important features of the immune system:
Unfortunately, when you have an autoimmune disease, your body’s immune system mistakenly confuses what is “self” with what is “other.” Instead of protecting your body, the immune system produces cells and chemicals that attack your own body, causing damage and disease.
There are many different autoimmune diseases, including psoriasis, rheumatoid arthritis, some types of thyroid diseases, some forms of anemia, lupus, celiac disease, and type 1 diabetes.
Don’t Miss: What Is Eczema And Psoriasis
What Exactly Is An Autoimmune Disease
When you have an autoimmune disease, your body mistakes normal, healthy tissues for foreign invaders. Basically, it goes to war with itself, causing damage and inflammation.
Not so fun fact: There are 100+ autoimmune diseases. Some of them, like psoriasis, only affects one body part . Others are system-wide, leaving your body exhausted and achy almost 24/7.
Regardless of your autoimmune diagnosis, your body is doing its war-waging thing because of some mysterious perfect storm of genetics and environmental factors.
Not Alone: Relations And Similarities Of Psoriasis With Other Autoimmune And Autoinflammatory Disorders
The highlights outlined so far show that both adaptive and innate immune processes contribute to psoriasis. Their balance and fine-tuning seem to determine the development of certain clinical forms of the disease, but also organ-specific manifestations. On the one hand, the outlined long-term systemic inflammatory processes probably contribute to the pathogenesis of important metabolic, cardiovascular, and mental concomitant diseases. In these areas, the evidence of a causal relationship is becoming increasingly clear and numerous publications prove this. A more detailed overview can be found elsewhere in this thematic focus. On the other hand, the contoured adaptive and innate immune mechanisms are not specific for psoriasis. Rather, many of them have been foundin varying degrees and weightingsin a whole range of other autoimmune and autoinflammatory diseases. In any case, although this interplay of different components of the immune system is certainly not yet fully understood, parallels with other chronic inflammatory and autoimmune diseases emerge that underpin our current view of psoriasis as a systemic disease.
Similar functional imbalances between Th17 and regulatory T cells as well as similar central cytokines including TNF, IL-23, and IL-17A, but also IL-1, IL-6, IL-17F, and IL-21 contribute to both diseases . Such striking parallels result in the response of both disorders to the same therapies.
Don’t Miss: Is Psoriasis A Communicable Disease