Rheumatoid Arthritis And Psoriasis
Around one-third of people with psoriasis develop a type of arthritis called psoriatic arthritis. This affects the joints and bones.
It is also possible for people to develop other types of arthritis, such as rheumatoid arthritis. Indeed, the risk of developing rheumatoid arthritis is higher in people with psoriasis than in people without.
However, many of the symptoms of rheumatoid arthritis and psoriatic arthritis overlap. This may mean that doctors avoid giving multiple diagnoses where one is enough.
Talk with your doctor if you think you are developing symptoms of rheumatoid arthritis or psoriatic arthritis, which include swelling and joint pain.
Treatments For Your Skin
If your psoriasis is affecting your quality of life, or your treatment is not working, you may be referred to a dermatologist.
There are a number of treatment options for psoriasis.
Ointments, creams, and gels that can be applied to the skin include:
- ointments made from a medicine called dithranol
- steroid-based creams and lotions
- vitamin D-like ointments such ascalcipotriol and tacalcitol
- vitamin A-like gels such astazarotene
- salicylic acid
- tar-based ointments.
For more information about the benefits and disadvantages of any of these talk to your GP, dermatologist, or pharmacist.
If the creams and ointments dont help, your doctor may suggest light therapy, also known as phototherapy. This involves being exposed to short spells of strong ultraviolet light in hospital.
Once this treatment has started, youll need to have it regularly and stick to the appointments youve been given, for it to be successful. This treatment is not suitable for people at high risk of skin cancer or for children. For some people, this treatment can make their psoriasis worse.
Retinoid tablets, such as acitretin, are made from substances related to vitamin A. These can be useful if your psoriasis isnt responding to other treatments. However, they can cause dry skin and you may not be able to take them if you have diabetes.
Some DMARDs used for psoriatic arthritis will also help with psoriasis.
Undertreatment Of Psoriasis Is Common
Dr. Yamauchi points out that many patients with moderate-to-severe psoriasis are undertreated. This may be less true of people with PsA, who now often begin therapy with a biologic however, diagnosis is often delayed, which is also an issue.
âIn psoriasis, undertreatment may happen because patients or providers arenât comfortable with biologics,â Dr. Yamauchi says. âSome think biologics are dangerous because thereâs the perception that they suppress the immune system. I explain that these agents target immune system pathways that contribute to psoriasis and its comorbidities and that biologics normalize them to control psoriatic disease and inflammation.â
Dr. Ogdie also emphasizes that treating psoriatic disease improves quality of life. âMany patients assume theyâre fine, but until their inflammation is under control, they donât know how good they can feel,â she says.
If your skin isnât clear or nearly clear, or you continue to have joint symptoms or fatigue from PsA that interferes with your daily life, your systemic inflammation may not be well-controlled, says Dr. Yamauchi.
Talk with your health care provider about medications that can bring your psoriatic disease â and the inflammation associated with it â under control.
Also Check: How To Stop Itching Scalp Psoriasis
Psoriasis = An Autoimmune Disease
Its taken years, but most researchers now classify psoriasis as an autoimmune disease. At the very least, they recognize a link between the two.
Its not hard to understand why. Folks with psoriasis have overactive T cells your immune systems personal fighter jets just like folks with other autoimmune diseases.
During a psoriasis flare-up, your T cells attack healthy skin cells with a special protein called cytokines. The cytokines make your skin cells multiply super fast so much so that they start building up on top of each other. This forms those dry, scaly patches.
In 2017, researchers confirmed that cytokines are involved in triggering psoriasis, which was a major milestone in the development of treatments.
Since then, research continues to indicate that immunosuppressants help with psoriasis.
Vitiligo Can Cause Skin To Lighten In Patches

Vitiligo causes your skin to lighten in patches as your body destroys melanocytes, the cells that make pigment. In some cases, your skin may lose all pigment and turn completely white. The condition can affect your hair, the inside of your mouth, and your eyes.
There is no cure for vitiligo, though treatments exist to restore pigment to the skin to even out your skin tone. These include cover-up or foundation, oral and topical medications, and light treatments applied to the affected areas. Light treatments can be time-intensive and costly, and they dont always work. Surgical treatments, such as skin grafting and tattooing, are another option.
Don’t Miss: Is Eating Oatmeal Good For Psoriasis
The Bodys Defenses Gone Rogue
Researcher Nehal N. Mehta, M.D., MSCE, is a senior investigator in the Section of Inflammation and Cardiometabolic Diseases at the National Heart, Lung, and Blood Institute in Bethesda, Maryland. For the past six years, he and other scientists in his NHLBI lab have followed a group of 350 people with plaque psoriasis, looking into how chronic inflammation affects their risk of heart disease and metabolic conditions such as diabetes.
âInflammation is simply a collection of immune cells trying to put out a fire, and that fire is usually an infection or some sort of virus,â says Dr. Mehta, a cardiologist and internist.
Setting off this inflammatory response, infiltration of immune cells and release of factors, is what the immune system evolved to do. In psoriatic disease, however, this primal defense has gone awry.
âIn psoriasis, immune cells attack places they shouldnât,â Dr. Mehta says. âThey go to the skin and cause psoriatic plaques, but they can also go to the joints and cause psoriatic arthritis. When they infiltrate blood vessels of the heart, they inflame the cells that line blood vessels. These fill with immune cells that donât belong there and cause inflammation. Thatâs the beginning of cardiovascular disease.â
How Do I Manage My Symptoms
- Take any OTC or prescription medications and products as recommended by your healthcare provider, including antihistamines for severe itching.
- Bathe or shower in lukewarm not hot water. Limit the amount of time you spend in the water to under 15 minutes and apply moisturizers or emollients immediately after lightly toweling dry.
- Use conditioner every time you wash your hair to keep your scalp and hair moisturized.
- Gently comb your hair to avoid causing irritation.
- Moisturize your scalp or affected areas several times a day using a cream or ointment, including after your bath or shower.
- Avoid wearing hats or other headwear unless necessary you generally dont want to cover your plaques so your scalp can breathe.
Don’t Miss: Is Aquaphor Good For Psoriasis
Links To Other Autoimmune Conditions
Having psoriasis means that you may have a higher risk of certain other autoimmune conditions and vice versa. Doctors refer to these conditions as comorbidities. One such example is psoriatic arthritis. As many as 33% of people with psoriasis also have psoriatic arthritis.
Other autoimmune conditions that have links with psoriasis include:
- mental health conditions
How Is Psoriasis Diagnosed And Treated
Psoriasis often has a typical appearance that a primary care doctor can recognize, but it can be confused with other skin diseases , so a dermatologist is often the best doctor to diagnose it. The treatment of psoriasis usually depends on how much skin is affected, how bad the disease is , or the location . Treatments range from creams and ointments applied to the affected areas to ultraviolet light therapy to drugs . Many people who have psoriasis also have serious health conditions such as diabetes, heart disease, and depression. Some people with psoriasis also have an inflammatory condition which affects their joints, called psoriatic arthritis.
Psoriatic arthritis has many of the same symptoms as other types of arthritis, so a rheumatologist is often the best doctor to diagnose it. The treatment of psoriatic arthritis usually involves the use of drugs .
Psoriatic disease may be treated with drugs or a combination of drugs and creams or ointments.
Don’t Miss: Salicylic Acid Lotion For Psoriasis
How Is Psoriasis Considered An Autoimmune Disease
For much of history, psoriasis has been seen as a disease of the skin. It is now clear that psoriasis is an autoimmune disease that impacts many systems of the body, involving multiple inflammatory pathways, with a primary presentation affecting the skin4. This inflammation can also affect the joints, vascular system, and eyes of people with psoriasis.
Psoriasis is the most common known human autoimmune disease, found in approximately 2-3% of the general population.
Several dozen gene locations have been identified that are believed to be involved in the development of psoriasis3. These genes are known to affect innate immunity, cell signaling processes, and skin barrier function.
These studies also provide more evidence that people with psoriasis may be genetically predisposed to other autoimmune diseases5.
With psoriasis, the body’s immune system goes haywire, sending out faulty signals that speed up the growth of skin. The way psoriasis affects the skin is primarily driven by a type of white blood cell called a T cell, as well as myeloid dendritic cells2. Normally, T cells help protect the body against foreign invaders.
Inflammatory myeloid dendritic cells release specific proteins to activate T cells. These T cells are then put into action by mistake and become so active that they trigger other immune responses, which lead to chronic inflammation and to the rapid turnover of skin cells5.
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else.
Psoriatic arthritis can be classed as a disability if it:
- makes daily tasks difficult
- lasts for more than 12 months.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
Don’t Miss: Is Baking Soda Good For Psoriasis
What Is Psoriatic Arthritis
Psoriatic arthritis is an autoimmune diseaseCLOSEAutoimmune disease: a disease that happens when a persons immune system attacks their own body. that affects different parts of the body. When this happens, you may experience various symptoms, including joint pain, swelling, and skin lesions. Sometimes these symptoms develop at the same time, and sometimes they can happen separately over a period of time. Read on to learn more about PsA.
In the U.S., as many as 329,000 adults have PsA
23.7million U.S. adults are limited in their activities by arthritis
PsA flares may also include heat, stiffness, and swelling
Why Do People Get Psoriasis
Both genetic and environmental factors are believed to be responsible for whether or not a person will get psoriasis. The theory is that those who develop the disease are born with a particular genetic makeup that causes vulnerability to psoriasis, and those who actually develop the disease are exposed to something in the environment that triggers the disorder.
Encountering certain environmental triggers seems to jump-start the machinery of the body’s immune system in vulnerable individuals. Some of the environmental factors that seem to be able to trigger psoriasis or to cause a flare-up of the condition in someone who already has the disorder include:
- Infections. Psoriasis often starts or worsens after you’ve had some kind of infection, especially one caused by streptococcus bacteria .
- Medications. Lithium, anti-malaria drugs, high blood pressure medicines and the anti-inflammatory drug Indocin are some of the drugs that seem to be possible triggers.
- Skin injury. Overly dry skin, sunburn, cuts, and scratches sometimes lead to psoriasis.
- Stress. Some studies suggest that stress can serve as a trigger for psoriasis.
Also Check: Link Between Psoriasis And Arthritis
How Are Autoimmune Diseases Treated
There are no cures for autoimmune diseases, but symptoms can be managed. Everyones immune system, genetics and environment are different. That means that your treatment must be unique.
Some examples of medications used to treat autoimmune diseases include:
- Painkillers.
- Limiting processed foods from your diet.
How Does Psoriatic Disease Affect The Immune System
Psoriatic disease is an immune-mediated disease that includes psoriasis, along with other comorbidities such as psoriatic arthritis and related systemic inflammation. In people living with psoriasis and/or PsA, the immune system is triggered and activated, acting as though there are harmful pathogens attacking the body.
This inflammation can present with noticeable signs such as discoloration of the skin or swelling around joints. However, the overactive immune system may also lead to inflammation a person cannot see. It can affect in the body, organs and systems and lead to other health conditions associated with psoriatic disease. Comorbidities of psoriatic disease include cardiovascular disease, metabolic syndrome, obesity, hypertension , type 2 diabetes, anxiety and depression, and more.
Researchers who study psoriatic disease are still working to identify the substances inside the body that trigger this immune response. One possibility could be certain kinds of bacteria acting as antigens . For example, sometimes streptococcal infection can trigger a case of guttate psoriasis. Another possible antigen could be antimicrobial peptides, molecules made by the body that are a part of the immune system and that work as antibiotics. *
Also Check: Psoriasis At Home Light Treatment
What Is Psoriatic Arthritis Video
Psoriatic arthritis can cause pain, swelling and stiffness inand around your joints.
It usually affects 3 in 10 people who already have the skin condition psoriasis .
Psoriasis causes patches of red, flaky skin which is covered with silvery-like patches.
Some people may develop psoriatic arthritis before the psoriasis is even present. In rare cases people have psoriatic arthritis and never have any noticeable patches of psoriasis.
Psoriatic arthritis and psoriasis are both autoimmune conditions, caused by a fault in the immune system.
Our immune system protects us from illness and infection. But in autoimmune conditions, the immune system becomes confused and attacks healthy parts of the body, often causing inflammation.
Psoriatic arthritis is a type of spondylarthritis. This is a group of conditions with some similar symptoms.
People with psoriasis are as likely as anyone else to get othertypes of arthritis, such asosteoarthritisorrheumatoid arthritis. Theseconditionsare not linkedto psoriasis.
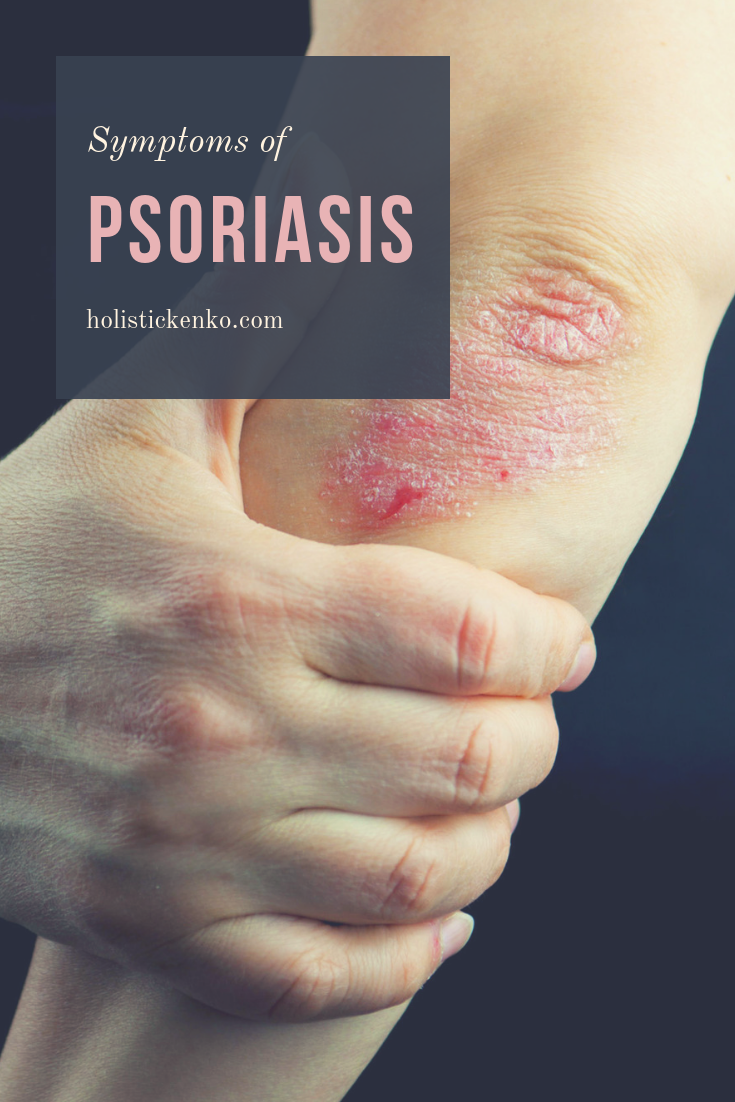
What Are The Symptoms Of Psoriasis
The following are the most common symptoms of psoriasis. Psoriasis comes in several forms and severities. Symptoms may include:
-
Plaque psoriasis. This type of psoriasis is the most common. Symptoms may include patches of red, raised skin on the trunk, arms, legs, knees, elbows, genitals, and scalp. Nails may also thicken, become pitted, and separate from the nail beds.
-
Guttate psoriasis. This type of psoriasis affects mostly children. Symptoms may include many small spots of red, raised skin. A sore throat usually proceeds the onset of this type of psoriasis.
-
Pustular psoriasis. Symptoms may include small pustules all over the body or just on the palms, soles, and other small areas.
The symptoms of psoriasis may look like other skin conditions. Always talk with your healthcare provider for a diagnosis.
Also Check: Eczema Vs Psoriasis On Hands
Lupus Can Cause A Rash Across The Nose And Cheeks
A butterfly-shaped rash across your nose and cheeks is the classic hallmark of lupus, an autoimmune disease that starts when your body attacks your organs and tissues and leads to inflammation. You may also experience lesions on your skin after sun exposure.
Treatments include nonsteroidal anti-inflammatory drugs, immunosuppressants, corticosteroids, and antimalarial drugs.
Why Psoriasis Is An Autoimmune Condition
Casey Gallagher, MD, is board-certified in dermatology and works as a practicing dermatologist and clinical professor.
Psoriasis causes a variety of symptoms that range from merely irritating to actually debilitating. The symptoms can include thick, red patches on the skin pitted, ridged fingernails scaly, itchy scalp and hair loss and stiff, painful joints.
Why do some people, but not others, get this frustrating condition in the first place? Arriving at an answer to this question relies partly on knowing that psoriasis is an autoimmune disorder “auto” meaning self and “immune” referring to the body’s complex immune system.
You May Like: Can Psoriasis Make Your Hair Fall Out
Should I Avoid Any Foods Or Drinks If I Have Scalp Psoriasis
Certain foods or drinks may contribute to scalp psoriasis flare-ups. If you have scalp psoriasis, its a good idea to keep track of what you eat and drink in a food journal. Keeping track of what you eat and drink can help you and your healthcare provider determine any causes of your flare-ups.
An anti-inflammatory diet may limit your scalp psoriasis flare-ups. Foods that have anti-inflammatory properties include:
- Oily fish, such as mackerel, salmon or sardines.
- Leafy greens, such as spinach and kale.
- Olive oil.
Foods and drinks that may cause flare-ups include:
- Alcohol.
- Dairy, including cows milk, and eggs.
- Citrus fruits, including lemons, limes and oranges.
- Gluten .
- Nightshade vegetables, including peppers, potatoes and tomatoes.