What Are The Symptoms Of Psoriasis
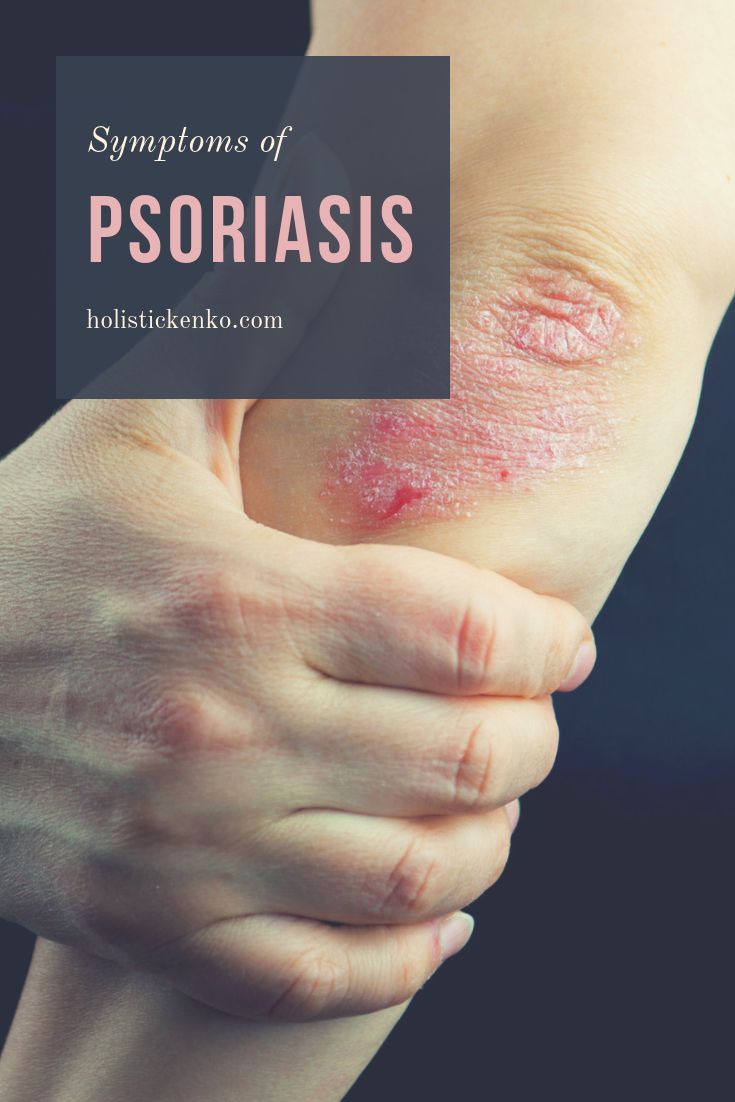
The following are the most common symptoms of psoriasis. Psoriasis comes in several forms and severities. Symptoms may include:
-
Plaque psoriasis. This type of psoriasis is the most common. Symptoms may include patches of red, raised skin on the trunk, arms, legs, knees, elbows, genitals, and scalp. Nails may also thicken, become pitted, and separate from the nail beds.
-
Guttate psoriasis. This type of psoriasis affects mostly children. Symptoms may include many small spots of red, raised skin. A sore throat usually proceeds the onset of this type of psoriasis.
-
Pustular psoriasis. Symptoms may include small pustules all over the body or just on the palms, soles, and other small areas.
The symptoms of psoriasis may look like other skin conditions. Always talk with your healthcare provider for a diagnosis.
Rheumatoid Arthritis And Psoriasis
Around one-third of people with psoriasis develop a type of arthritis called psoriatic arthritis. This affects the joints and bones.
It is also possible for people to develop other types of , such as rheumatoid arthritis. Indeed, the risk of developing rheumatoid arthritis is higher in people with psoriasis than in people without.
However, many of the symptoms of and psoriatic arthritis overlap. This may mean that doctors avoid giving multiple diagnoses where one is enough.
Talk with your doctor if you think you are developing symptoms of rheumatoid arthritis or , which include swelling and .
How Is Psoriasis Considered An Autoimmune Disease
For much of history, psoriasis has been seen as a disease of the skin. It is now clear that psoriasis is an autoimmune disease that impacts many systems of the body, involving multiple inflammatory pathways, with a primary presentation affecting the skin4. This inflammation can also affect the joints, vascular system, and eyes of people with psoriasis.
Psoriasis is the most common known human autoimmune disease, found in approximately 2-3% of the general population.
Several dozen gene locations have been identified that are believed to be involved in the development of psoriasis3. These genes are known to affect innate immunity, cell signaling processes, and skin barrier function.
These studies also provide more evidence that people with psoriasis may be genetically predisposed to other autoimmune diseases5.
With psoriasis, the body’s immune system goes haywire, sending out faulty signals that speed up the growth of skin. The way psoriasis affects the skin is primarily driven by a type of white blood cell called a T cell, as well as myeloid dendritic cells2. Normally, T cells help protect the body against foreign invaders.
Inflammatory myeloid dendritic cells release specific proteins to activate T cells. These T cells are then put into action by mistake and become so active that they trigger other immune responses, which lead to chronic inflammation and to the rapid turnover of skin cells5.
Don’t Miss: Psoriasis Hair Loss Grow Back
Should I Avoid Any Foods Or Drinks If I Have Scalp Psoriasis
Certain foods or drinks may contribute to scalp psoriasis flare-ups. If you have scalp psoriasis, its a good idea to keep track of what you eat and drink in a food journal. Keeping track of what you eat and drink can help you and your healthcare provider determine any causes of your flare-ups.
An anti-inflammatory diet may limit your scalp psoriasis flare-ups. Foods that have anti-inflammatory properties include:
- Oily fish, such as mackerel, salmon or sardines.
- Leafy greens, such as spinach and kale.
- Olive oil.
Foods and drinks that may cause flare-ups include:
- Alcohol.
- Dairy, including cows milk, and eggs.
- Citrus fruits, including lemons, limes and oranges.
- Gluten .
- Nightshade vegetables, including peppers, potatoes and tomatoes.
Psoriasis = An Autoimmune Disease
Its taken years, but most researchers now classify psoriasis as an autoimmune disease. At the very least, they recognize a link between the two.
Its not hard to understand why. Folks with psoriasis have overactive T cells your immune systems personal fighter jets just like folks with other autoimmune diseases.
During a psoriasis flare-up, your T cells attack healthy skin cells with a special protein called cytokines. The cytokines make your skin cells multiply super fast so much so that they start building up on top of each other. This forms those dry, scaly patches.
In 2017, researchers confirmed that cytokines are involved in triggering psoriasis, which was a major milestone in the development of treatments.
Since then, research continues to indicate that immunosuppressants help with psoriasis.
Don’t Miss: Is Psoriasis Caused By A Virus
How Does It Affect Psoriasis Treatment Options
The primary goals of treatment are to:
- Reduce symptoms
- Control the autoimmune process
- Maintain the body’s ability to fight disease
For people with moderate to severe plaque psoriasis, an immunosuppressive drug may be needed to reduce their immune system’s abnormal responses. Your healthcare provider may prescribe medication that is designed to affect processes of inflammation throughout your entire body, like a corticosteroid.
In other cases, your healthcare provider may choose a therapeutic biologic medication that is designed to target a specific inflammatory pathway.
Combining biologics with traditional psoriasis therapies may provide an important treatment option for people who do not adequately respond to monotherapy. These approaches are called combination therapy.
Combination therapy may also help in the prevention or treatment of co-occurring diseases in certain patients.
One concern of patients considering biologics for treatment of psoriasis is it may increase their risk of infection. However, it is important to note that much of the available data regarding susceptibility to infection with biologic therapy derives from studies in inflammatory diseases other than psoriasis, such as rheumatoid arthritis and Crohns disease.
What Is An Autoimmune Disease
In an autoimmune disease, the body loses the ability to tell the difference between some of the bodys tissues and harmful microbes that can cause sickness, leading the body to attack healthy tissue.
The immune system is made up of cells and proteins that attack anything foreign to the body, such as invading bacteria, viruses, and other potential causes of infection and sickness. The immune system is designed to attack and neutralize invaders by recognizing molecules on them known as antigens. It is important that the immune system knows the difference between the bodys own tissues and a foreign invader.
However, when immune cells begin responding abnormally, they misidentify aspects of our own body as harmful invaders and attack. This abnormal response is described as being autoreactive or autoimmune auto is a Greek prefix meaning self. The self-antigens targeted in autoimmune diseases are known as autoantigens.
Autoimmune diseases are classified by the type of tissue that is being attacked. For example, in rheumatoid arthritis, the tissue lining the inside of the joints is attacked. In type 1 diabetes, the immune system attacks and destroys insulin-producing cells in the pancreas. In celiac disease, the immune system attacks the small intestine when gluten is consumed. And in people with psoriasis, the immune system produces inflammatory reactions against molecules related to the skin.
Don’t Miss: Treatments For Plaque Psoriasis Scalp
The Role Of Inflammation
Inflammation is an important reaction to infection, injuries, and toxins. When the immune response of the body is triggered in cases of psoriatic disease, it can lead to inflammation that can cause skin and/or joint symptoms to flare , along with systemic inflammation that can affect other parts of the body.
Normally, it takes 21 to 28 days for cells on the surface of the skin to grow and shed it may take as few as four days in skin affected by psoriasis, due to the increased immune response. For psoriasis, a flare may include new psoriasis plaques or the return of plaques to a prior location, itch, irritation, or burning.
With PsA, a flare may include new or increased pain, tenderness, swelling, or stiffness in joints. Flares may last for various amounts of time and may vary in level of severity.
However, having skin affected by psoriasis or joints affected by PsA can be a sign of inflammation occurring in other parts of the body. Even people living with mild psoriasis may have inflammation in the body.
What Exactly Is An Autoimmune Disease
When you have an autoimmune disease, your body mistakes normal, healthy tissues for foreign invaders. Basically, it goes to war with itself, causing damage and inflammation.
Not so fun fact: There are 100+ autoimmune diseases. Some of them, like psoriasis, only affects one body part . Others are system-wide, leaving your body exhausted and achy almost 24/7.
Regardless of your autoimmune diagnosis, your body is doing its war-waging thing because of some mysterious perfect storm of genetics and environmental factors.
Read Also: How To Treat Psoriasis On Hands
The Impact Of Psoriatic Disease Comorbidities
Psoriasis and PsA, and the comorbidities they lead to, can shorten your life. âPeople with psoriasis tend to live a few years less than those without the condition. This is particularly true for those with severe disease,â says Dr. Yamauchi. âItâs not the psoriasis thatâs shortening life span, but the heart attacks, strokes and other comorbidities it can cause.â
Letâs look at how some common comorbidities of psoriatic disease can affect your life and health.
Not Alone: Relations And Similarities Of Psoriasis With Other Autoimmune And Autoinflammatory Disorders
The highlights outlined so far show that both adaptive and innate immune processes contribute to psoriasis. Their balance and fine-tuning seem to determine the development of certain clinical forms of the disease, but also organ-specific manifestations. On the one hand, the outlined long-term systemic inflammatory processes probably contribute to the pathogenesis of important metabolic, cardiovascular, and mental concomitant diseases. In these areas, the evidence of a causal relationship is becoming increasingly clear and numerous publications prove this. A more detailed overview can be found elsewhere in this thematic focus. On the other hand, the contoured adaptive and innate immune mechanisms are not specific for psoriasis. Rather, many of them have been foundin varying degrees and weightingsin a whole range of other autoimmune and autoinflammatory diseases. In any case, although this interplay of different components of the immune system is certainly not yet fully understood, parallels with other chronic inflammatory and autoimmune diseases emerge that underpin our current view of psoriasis as a systemic disease.
Similar functional imbalances between Th17 and regulatory T cells as well as similar central cytokines including TNF, IL-23, and IL-17A, but also IL-1, IL-6, IL-17F, and IL-21 contribute to both diseases . Such striking parallels result in the response of both disorders to the same therapies.
Also Check: How To Treat Psoriasis On Lips
What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
Screen For And Treat Comorbidities

If you have psoriasis, your dermatologist or primary care physician should screen you regularly â at least once a year â for PsA, says Dr. Ogdie.
âThe earlier you catch it and start treatment, the more likely you are to respond to therapy,â she says, noting that early treatment also potentially lowers the chances of permanent joint damage.
Dr. Ogdie advises people with psoriasis to understand the signs and symptoms of PsA. These include joint pain, swelling and tenderness â particularly in fingers and toes â and enthesitis, or inflammation at the points where tendons insert into bones. In addition, having psoriasis in the nails, scalp or skinfolds should raise suspicion for PsA, as should a family history of the disease.
âIf you have new symptoms, tell your doctor,â Dr. Ogdie says. âRemind them you have psoriasis and ask if these changes could mean you have psoriatic arthritis.â
Comorbidities such as CVD and metabolic syndrome can start developing at young ages in people with psoriasis and PsA, and sometimes health care providers arenât looking for them, Dr. Mehta says.
âPeople with psoriasis should ask their doctors to screen them for heart and metabolic disease. They can do this by checking the three âBs,â which are blood pressure, body mass index and blood levels of glucose and cholesterol,â he says.
You May Like: Which Treatment Is Better For Psoriasis Homeopathy Or Allopathy
What Are The Four Categories Of Immune System Disorders
You may:
- Be born with a weak immune system. This is called primary immune deficiency.
- Get a disease that weakens your immune system. This is called acquired immune deficiency.
- Have an immune system that is too active. This may happen with an allergic reaction.
- Have an immune system that turns against you.
Setting The Stage: Psoriasis As An Immune
Figure 1. Complex fine-tuning of innate and adaptive immune mechanisms determines onset, course, and activity of psoriasis. As detailed in the text, intricate interactions between components of the innate with components of the adaptive immune system lie at the core of the pathophysiology of psoriasis. Once established, the relative contribution and fine-tuning of various mediators of adaptive and innate immunity determine the clinical manifestation toward chronic stable vs. highly inflammatory and/or pustular psoriasis.
Don’t Miss: Does Olive Oil Help Psoriasis
Links To Other Autoimmune Conditions
Having psoriasis means that you may have a higher risk of certain other autoimmune conditions and vice versa. Doctors refer to these conditions as comorbidities. One such example is psoriatic arthritis. As many as 33% of people with psoriasis also have psoriatic arthritis.
Other autoimmune conditions that have links with psoriasis include:
- mental health conditions
Treatments That Target The Immune System
Treatment for psoriasis depends on the type and severity of the condition, your general health, and other factors.
Here are the various treatments that target specific factors in the immune system that cause inflammation. These are generally used when your psoriasis symptoms are moderate to severe. Note that the newer drugs are more expensive.
You May Like: Natural Shampoo For Scalp Psoriasis
Psoriasis Association With Other Autoimmune Diseases
Association of psoriasis with other autoimmune diseases is an ongoing research area. Previous studies have shown that there is a higher frequency of autoimmune diseases among psoriasis patients than observed in the general population potentially stemming from cytokine pathways dysregulation., Based on a retrospective study using MEDLINE data from January 1, 1980 to June 1, 2011, the major autoimmune disorders associated with psoriasis include RA, celiac disease, IBD, especially CD, multiple sclerosis, SLE, and autoimmune thyroid disease. However, anecdotal reports of other autoimmune diseases associated with psoriasis include Sjögrens syndrome and alopecia areata. In addition, a new meta-analysis of a single mutation of CD226, Gly307Ser has suggested that this modification is associated with an increased risk of developing various autoimmune disorders including psoriasis.
Why Is Psoriasis An Autoimmune Disorder
As part of its defense against foreign invaders, your body makes specialized white blood cells called T-cells. Under normal circumstances, T-cells identify and coordinate attacks on foreign invaders.
However, when you have psoriasis, your T-cells mistakenly identify your skin cells as invaders and attack them. This attack injures the skin cells, setting off a cascade of responses in your immune system and in your skin, resulting in the skin damage seen in psoriasis swelling, reddening, and scaling.
In an effort to heal, your skin cells begin reproducing much more rapidly than normal, and large numbers of new skin cells push their way to the surface of your skin. This occurs so quickly that older skin cells and white blood cells aren’t shed quickly enough. These discarded cells pile up on the surface of the skin, creating thick, red plaques with silvery scales on their surface: the hallmark of the classic form of plaque psoriasis.
Read Also: Ways To Get Rid Of Psoriasis
Is Psoriasis Autoimmune
Psoriasis is an autoimmune disease because it happens due to the immune system attacking its own healthy cells. It also has links with other autoimmune conditions.
In a person with psoriasis, the immune system does not function as it should. T cells, which the body uses to fight potentially dangerous substances in the body such as harmful bacteria that could make us sick begin to attack healthy skin cells.
Because the body is attacking these cells, it begins to make new cells to replace the ones that the immune system has destroyed. This causes an imbalance in the life cycle of the cells, which means that skin cells build up on the skin. This causes a scaly rash.
What Is Psoriasis

Psoriasis is a skin disease that causes itchy or sore patches of thick, red skin with silvery scales. You usually get the patches on your elbows, knees, scalp, back, face, palms and feet, but they can show up on other parts of your body. Some people who have psoriasis also get a form of arthritis called psoriatic arthritis. A problem with your immune system causes psoriasis. In a process called cell turnover, skin cells that grow deep in your skin rise to the surface. Normally, this takes a month. In psoriasis, it happens in just days because your cells rise too fast. Psoriasis can be hard to diagnose because it can look like other skin diseases. Your doctor might need to look at a small skin sample under a microscope. Psoriasis can last a long time, even a lifetime. Symptoms come and go. Things that make them worse include: infections, stress, dry skin, and certain medicines. Psoriasis usually occurs in adults. It sometimes runs in families. Treatments include creams, medicines, and light therapy.
Read Also: Plaque Psoriasis And Psoriatic Arthritis