Risk Factors For Developing Psoriatic Arthritis
Several factors can increase your risk of developing psoriatic arthritis.5,6
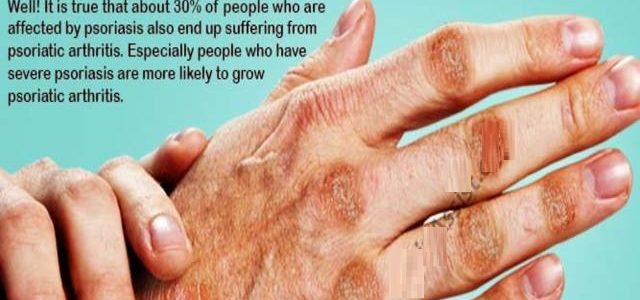
- Psoriasis. Having psoriasis is the single greatest risk factor for developing psoriatic arthritis. People who have pitted, deformed nails are especially likely to develop psoriatic arthritis.
- Your family history. While its not clear why the body attacks healthy tissue in patients with psoriatic disease, there is likely a genetic component. People living with plaque psoriasis or psoriatic arthritis often have a family member with the disease.
- Your age. Psoriatic arthritis most often occurs in adults between the ages of 30 and 50. Men and women are equally at risk.
Connecting Psoriasis And Psoriatic Arthritis
Psoriatic arthritis is very similar to psoriasis. Both involve healthy cells attacking the immune system. But, rather than plaques forming or skin flaking off, psoriatic arthritis affects the joints and causes them to swell and become painful.
Psoriatic arthritis can also get worse if its left untreated. According to the health service in the UK, its not clear why some people develop psoriatic arthritis, while others do not. Having psoriasis alone can be enough of a problem for me. I am currently on a biologic injection which, at times after administering, does cause me some problems with fatigue, tiredness, and exhaustion.
However, I am aware that there are plenty of treatment options available for psoriatic arthritis like biologics, just as there are with psoriasis.
Summary Plaque Psoriasis Vs Psoriasis
Psoriasis is a chronic multisystem disease with skin and joint manifestations. Plaque psoriasis is the commonest form of psoriasis which is characterized by the appearance of reddish well-demarcated plaques with silver scales usually on the extensor surface of the knees and elbows. Accordingly plaque psoriasis is one manifestation of the broad spectrum of dermatological and systemic manifestations which are identified as psoriasis. This can be identified as the difference between plaque psoriasis and psoriasis.
Read Also: Best Shampoo Bar For Psoriasis
Lifestyle Changes Can Help
If you have PsO, there are things you can do to try to lower your chances of developing PsA, too. One modifiable risk factor is being overweight or obese, says Dr. Orbai. A possible explanation is that there might be more wear and tear on joints when someone is carrying more weight, which leads to inflammation. It could also be because inflammation is amplified by the fatty cells in the tissue.
Regular exercise and smart food choices based on the Mediterranean diet can help you reach a healthy weight and lower inflammation in your body.
Other ways to reduce your chances of developing PsA? If you smoke, quit. Moderate your alcohol intake, avoid cold weather , and find ways to boost your mood: A 2017 Canadian study found that psoriasis patients who reported depression were at a 37% greater risk of developing psoriatic arthritis.
Treatment Options For Both Psoriasis And Psa
Drugs to suppress immune system activity are among the most effective treatments for psoriasis and PsA.
Systemic, immune-suppressing drugs often provide relief for both conditions. However, your risk of secondary infections and other side effects is greater when using these drugs.
If you have severe psoriasis and are diagnosed with PsA, your doctor may prescribe the anti-inflammatory and immune-suppressant drug methotrexate . This medication aims to slow down the cells in your body that are reproducing too quickly and causing psoriasis flares.
Common side effects of methotrexate include:
- headaches
- dizziness
- upset stomach
A newer class of drugs called biologics, in particular TNF blockers, targets specific parts of the immune system more precisely. Because of this, your doctor may be more likely to recommend them over methotrexate.
Biologics reduce inflammation and psoriasis outbreaks in most people who take them. There are a number of brands of biologics approved for treatment of psoriasis in the United States.
Biologics need to be injected. Some need to be administered more often than others. Common side effects include:
- allergic reaction
Don’t Miss: Scalp Psoriasis On Black Skin
Find Comfort In Community
It would also be helpful to speak to people with the condition. Luckily, Health Union has a great psoriatic arthritis community which can really help with that. But, if you want more, there are lots of people on Facebook, Twitter, and Instagram who post about living with psoriatic arthritis and the daily challenges they face with the condition. It can be a real eye-opener reading their stories and seeing how psoriatic arthritis affects them.
While researching, try to keep an open mind. Comorbidities can affect people in different ways. You may have a severe version of psoriasis, but only develop a mild or moderate case of psoriatic arthritis. You may have a mild or moderate version of psoriasis, but develop severe symptoms of psoriatic arthritis.
As Ive said throughout this piece, there are plenty of medications available. Its important therefore to get a sense of perspective and try to persevere. You dont know what the future holds.
Psoriatic Arthritis And Psoriasis Are Both Autoimmune Conditions
Both conditions happen when your autoimmune system mistakenly attacks healthy cells in your body, causing inflammation. With psoriasis, new skin cells grow too quickly and build up, resulting in thick, scaly rashes that can make it painful to move, according to the Cleveland Clinic. People with psoriatic arthritis also have inflammation, but their symptoms generally result in stiff, painful joints, and swollen skin surrounding the joints, according to the Mayo Clinic.
The exact causes of autoimmune diseases are not clear. Some experts theorize that injuries might trigger psoriatic arthritis and that infections could trigger psoriasis, according to John Hopkins University. Doctors commonly suspect that genetics may determine whether someone is susceptible to autoimmune disorders, but the specifics explaining how or why are up in the air.
Both conditions are lifelong diseases that can alternate between periods of remission where you have very few symptoms and flares in which your symptoms are worse.
Don’t Miss: What Vitamins Can Help Psoriasis
Can Psoriatic Arthritis Affect Other Parts Of The Body
Having psoriatic arthritis can put you at risk of developing other conditions and complications around the body.
The chances of getting one of these are rare. But its worth knowing about them and talking to your doctor if you have any concerns.
Eyes
Seek urgent medical attention if one or both of your eyes are red and painful, particularly if you have a change in your vision. You could go to your GP, an eye hospital, or your local A& E department.
These symptoms could be caused by a condition called uveitis, which is also known as iritis. It involves inflammation at the front of the eye.
This can permanently damage your eyesight if left untreated.
Other symptoms are:
- blurred or cloudy vision
- sensitivity to light
- not being able to see things at the side of your field of vision known as a loss of peripheral vision
- small shapes moving across your field of vision.
These symptoms can come on suddenly, or gradually over a few days. It can affect one or both eyes. It can be treated effectively with steroids.
Heart
Psoriatic arthritis can put you at a slightly higher risk of having a heart condition. You can reduce your risk by:
- not smoking
- staying at a healthy weight
- exercising regularly
- eating a healthy diet, thats low in fat, sugar and salt
- not drinking too much alcohol.
These positive lifestyle choices can help to improve your arthritis and skin symptoms.
Talk to your doctor if you have any concerns about your heart health.
Crohns disease
Non-alcoholic fatty liver disease
Sex Fertility And Pregnancy
Sex can sometimes be painful for people with psoriatic arthritis, particularly a woman whose hips are affected. Experimenting with different positions and communicating well with your partner will usually provide a solution.
Psoriatic arthritis wont affect your chances of having children. But if youre thinking of starting a family, its important to discuss your drug treatment with a doctor well in advance. If you become pregnant unexpectedly, talk to your rheumatology department as soon as possible.
The following must be avoided when trying to start a family, during pregnancy and when breastfeeding:
Recommended Reading: Light Therapy For Psoriasis At Home
There Are Many Treatment Options Available To People With Psoriasis And Psoriatic Arthritis It Can Seem Overwhelming But It Sure Beats Not Having Enough Options
Mild psoriasis is typically treated with creams, ointments, and lotions applied directly to the skin, most often with topical steroids. Mild psoriasis treatments are examined here. Those with moderate or severe psoriasis also sometimes use such topical treatments, particularly for stubborn psoriasis patches or other hard-to-treat areas.
But most moderate to severe psoriasis and psoriatic arthritis is treated with treatments that impact the whole body: ultraviolet lights directed at the skin, pills that are taken by mouth, injections made under the skin, and infusions directly into the bloodstream.
Today patients can select treatments that are more effective, more safe, and able to be used longer than ever before. We review these options below.
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else. Psoriatic arthritis can be classed as a disability if its making every-day tasks difficult.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
Also Check: How To Stop Guttate Psoriasis Spreading
Symptoms Of Psoriatic Arthritis
Psoriatic arthritis occurs when the immune system attacks healthy cells in the body. This abnormal immune response causes inflammation of the joints and can also lead to an overproduction of skin cells. Psoriatic arthritis is sometimes confused with other forms of arthritis including rheumatoid arthritis and osteoarthritis. Below are the common symptoms of each. 4,5
Efficacy And Safety Of Biologics

Although approved biologic agents differ by countries, biologic agents commonly used for the treatment of psoriasis are categorized into three groups, tumor necrosis factor – inhibitors, interleukin -23 inhibitors, and IL-17 inhibitors, as shown in . Infliximab, adalimumab, etanercept, certolizumab-pegol, and golimumab are TNF- inhibitors. Golimumab is used only for PsA. Ustekinumab is an anti-IL-12/23p40 antibody. Guselkumab, risankizumab, tildrakizumab, and mirikizumab are anti-IL-23p19 antibodies. Secukinumab, and ixekizumab are anti-IL-17A antibodies. Brodalumab is an anti-IL-17RA antibody. Bimekizumab is an anti-IL-17A/F antibody, which blocks both IL-17A and IL-17F. Many randomized controlled trials were conducted, and they demonstrated that the drugs are efficacious for moderate-to-severe plaque psoriasis. Recently, network meta-analyses enabled indirect comparison among those agents.
Don’t Miss: Scalp Psoriasis And Psoriatic Arthritis
Main Cytokines And Cell Types In Plaque Psoriasis
Disturbances in the innate and adaptive cutaneous immune responses are responsible for the development and sustainment of psoriatic inflammation . An activation of the innate immune system driven by endogenous danger signals and cytokines characteristically coexists with an autoinflammatory perpetuation in some patients, and T cell-driven autoimmune reactions in others. Thus, psoriasis shows traits of an autoimmune disease on an inflammatory background , with both mechanisms overlapping and even potentiating one another.
The main clinical findings in psoriasis are evident at the outermost layer of the skin, which is made up of keratinocytes. However, the development of the psoriatic plaque is not restricted to inflammation in the epidermal layer, but rather is shaped by the interaction of keratinocytes with many different cell types spanning the dermal layer of the skin. The pathogenesis of psoriasis can be conceptualized into an initiation phase possibly triggered by trauma , infection, or drugs and a maintenance phase characterized by a chronic clinical progression .
The pathogenesis of psoriasis.
The activation of the adaptive immune response via the distinct T cell subsets drives the maintenance phase of psoriatic inflammation . Th17 cytokines, namely IL-17, IL-21, and IL-22 activate keratinocyte proliferation in the epidermis.
Evaluation And Differential Diagnosis
Less common variants of psoriasis include inverse psoriasis, pustular psoriasis, guttate psoriasis, erythrodermic psoriasis, and annular psoriasis .6). These variants can be differentiated from the common plaque type by morphology. Differential diagnoses include atopic dermatitis, contact dermatitis, lichen planus, secondary syphilis, mycosis fungoides, tinea corporis, and pityriasis rosea . Careful observation often yields the diagnosis. For more atypical presentations, a skin biopsy might be helpful.
Differential diagnoses and distinguishing clinical features
| DIFFERENTIAL DIAGNOSES | DISTINGUISHING CLINICAL FEATURES |
|---|---|
| Atopic dermatitis | Predominant symptom of pruritus and typical morphology and distribution |
| Contact dermatitis | Patches or plaques with angular corners, geometric outlines, and sharp margins dependent on the nature of the exposure to the irritant or allergen |
| Lichen planus | Violaceous lesions and frequent mucosal involvement |
| Secondary syphilis | Copper-coloured lesions and frequent involvement of palms and soles |
| Mycosis fungoides | Irregularly shaped lesions with asymmetric distribution, peculiar colour, and wrinkling due to epidermal atrophy |
| Tinea corporis | Fewer lesions with annular configuration |
| Pityriasis rosea | Tannish-pink, oval papules and patches with Christmas tree configuration on trunk with sparing of the face and distal extremities |
You May Like: Skin Care Routine For Psoriasis
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
How Is Psoriasis Diagnosed And Treated
Psoriasis often has a typical appearance that a primary care doctor can recognize, but it can be confused with other skin diseases , so a dermatologist is often the best doctor to diagnose it. The treatment of psoriasis usually depends on how much skin is affected, how bad the disease is , or the location . Treatments range from creams and ointments applied to the affected areas to ultraviolet light therapy to drugs . Many people who have psoriasis also have serious health conditions such as diabetes, heart disease, and depression. Some people with psoriasis also have an inflammatory condition which affects their joints, called psoriatic arthritis.
Psoriatic arthritis has many of the same symptoms as other types of arthritis, so a rheumatologist is often the best doctor to diagnose it. The treatment of psoriatic arthritis usually involves the use of drugs .
Psoriatic disease may be treated with drugs or a combination of drugs and creams or ointments.
You May Like: What Does Psoriasis Look Like When It First Appears
What Causes Psoriasis And Psoriatic Arthritis
The symptoms of both psoriasis and psoriatic arthritis arise when the bodys immune system malfunctions, leading to inflammation.
In psoriasis, the faulty reaction causes skin cells to grow too fast, promoting a buildup of skin cells on the surface. These cells appear as a scaly rash.
In psoriatic arthritis, the inflammation affects the joints. Permanent damage can result if the person does not seek treatment.
Doctors do not yet know the exact causes of psoriasis and psoriatic arthritis. However, they do know that genetics contribute to both conditions.
An estimated 1 out of 3 people with psoriasis say that they have a family member with psoriasis. Also, around 40 percent of people with psoriatic arthritis have a family member with psoriatic disease.
Still, many people have genes for psoriatic disease and never develop it. To develop psoriatic disease, a person must have the specific genes for it, as well as a trigger that activates it.
Possible triggers for psoriatic disease include:
- an infection, such as strep throat or a cold
- use of tobacco or smoking
- heavy alcohol use
These triggers may bring on psoriasis, and they can also cause flares. Flares are cycles during which symptoms become worse. Triggers vary from person to person and may change over time.
Psoriasis and psoriatic arthritis symptoms often come and go in cycles. They may get worse during a flare and then improve. Symptoms may also move around, affecting different areas of the body at different times.