Role Of Family Physicians In Psoriasis Management
Even though the majority of psoriasis patients may be managed with topical medication, nonadherence rates for topical treatment is estimated at 40%,18 including up to 50% for unfilled prescriptions.19
As the primary contact for people seeking healthcare, family physicians play a crucial role in promoting treatment adherence among psoriasis patients. This may be achieved by adopting a more patient-specific approach to management, through engaging in ongoing discussions with patients about treatment expectations, choice of therapy, including offering simplified dosing regimens, as well as regularly assessing tolerability and side-effects from medications.
Role Of Vitamin D In Skin Physiology
Vitamin D plays a vital role in the skin: the keratinocytes are not only a source of vitamin D, but also a responder to its active form . They are the only cells in the body that can synthesize vitamin D from its precursor 7-DHC, and which are equipped with the entire enzymatic machinery necessary to metabolize vitamin D into its active metabolite 1,252D. Keratinocytes also express VDR, thus they respond in an autocrine and paracrine manner to the active form of vitamin D. The entire pathway of vitamin D3 in human skin is shown in Figure 1.
Fig. 1
Summary of vitamin D3 pathway and functions in the human skin. Vitamin D3 is synthesized in the skin from its precursor 7-DHC under the influence of UVB and metabolized to its active form, 1,252D3 through 2 subsequent hydroxylation reactions by CYP27A1 and CYP27B1 enzymes. It is rendered inactive through the catabolic enzyme CYP24A1. 7-DHC, 7-dehydrocholesterol 25D3, 25-hydroxyvitamin D3 1,252D3, 1,25-dihydroxyvitamin D3 24,252D3, 24,25-dihydroxycholecalciferol 1,24,253D3, 1,24,25-trihydroxycholecalciferol CYP27A1, 25-hydroxylase CYP27B1, 1-hydroxylase CYP24A1, 24-hydroxylase AMP, antimicrobial peptide Ag, antigen UVB, ultraviolet radiation B.
How Can Vitamin D Benefit People With Psoriasis
Vitamin D which is often made in a layer of the skin called the epidermis plays an important role in skin health. Research shows that people with psoriasis tend to have lower levels of vitamin D. Low levels of the nutrient can increase skin-cell proliferation, which can contribute to psoriasis lesions. On the other hand, high doses of vitamin D have been shown to reduce skin-cell proliferation and inflammation.
Vitamin D treatments may be taken orally or applied directly to the skin.
Read Also: Psoriasis On Scalp African American
Vitamin D Regulation Of Apoptosis In Keratinocytes
Calcitriol stimulates the synthesis of ceramide by inducing the neutral Mg2+-dependent sphingomyelinase and in return, ceramide enhances the pro-differentiating effect of calcitriol on keratinocytes in a feedback loop . It has been demonstrated that physiological concentrations of calcitriol do not initiate apoptosis in cultured keratinocytes but, in contrast, pharmacological concentrations of calcitriol exert a pro-apoptotic effect on keratinocytes .
Cell Culture And Stimuli
Normal human epidermal keratinocytes were grown in EpiLife® cell culture medium containing 0.06 mM calcium and 1 x EpiLife® defined growth supplement at 37°C under standard tissue culture conditions. Stock cultures were maintained for up to six passages in this medium with the addition of 10 µg/ml gentamicin and 0.25 µg/ml amphotericin B. HaCaT keratinocytes were cultured in Dulbecco’s modified Eagle’s medium with 4.5 g/l glucose supplemented with 10% fetal bovine serum, 50 U/ml penicillin and 50 µg/ml streptomycin . Cells at 4060% confluence were stimulated for different time periods with 1,25-dihydroxyvitamin D3 , calcipotriol , ZK159222 , ZK191784 , ZK203278 and/or IL-17A . For inhibition of MEK/ERK the MEK1 inhibitor PD98059 was added 1 h before stimulation.
Don’t Miss: Inverse Psoriasis Or Jock Itch
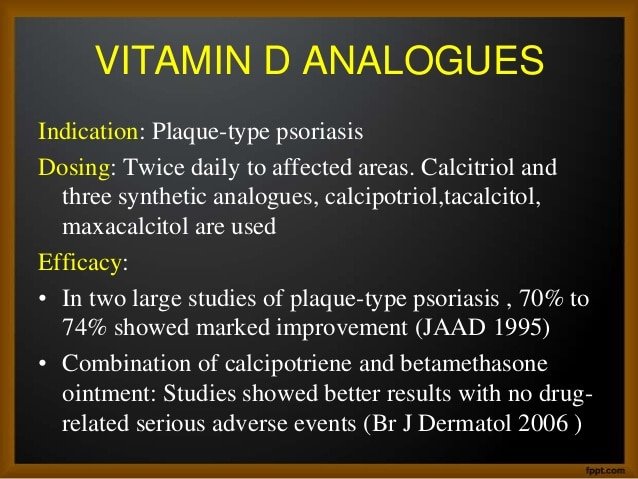
The Rationale Behind Topical Vitamin D Analogs In The Treatment Of Psoriasis
Topical vitamin D analogs have become an integral component of the armamentarium used for the treatment of psoriasis. Clinical experience and multiple studies with topical vitamin D analogs have demonstrated efficacy with both monotherapy and combination therapy, with the latter approach found to be more applicable in the clinical setting. The most recent of this class of agents released in the United States is calcitriol. Calcitriol is a natural topical vitamin D3 analog with both short- and long-term studies demonstrating its efficacy and safety, with minimal risk of side effects., Studies have confirmed its efficacy as monotherapy however, this agent is also applicable to combination therapy for psoriasis, providing a corticosteroid-sparing benefit with a reduction in side effects and a decrease in relapse rates. The following review provides an overview of psoriasis management, with a focus on the use of topical therapy, and examines the evolution of calcitriol ointment in psoriasis treatment. Emphasis is placed primarily on the management of chronic plaque psoriasis.
Definition Of Inclusion And Exclusion Criteria
- prospective trials on adult subjects
- trials on patients with plaque psoriasis of the trunk and the extremities and/or the scalp excluding psoriasis pustulosa and erythrodermic psoriasis
- trials, which only evaluated topical therapy with a vitamin D3 analogue, a corticosteroid or a fixed or free combination of both
- trials, in which topical therapy is used as continuous maintenance therapy
- trials with a treatment duration of at least 24 weeks
- trials, in which a validated, reproducible score-based efficacy measure was used, if efficacy was the primary end point
- trial reports in German or English
Also Check: Are Tanning Beds Good For Psoriasis
Vitamin D Analogs Induce Cathelicidin Expression In Human Keratinocytes
Cathelicidin is another antimicrobial peptide which acts as an alarmin in skin. In particular, cathelicidin peptide LL-37 has been identified as a critical factor for the activation of an inflammatory cascade in psoriasis . Unexpectedly, despite clinical improvement and a decrease in inflammatory parameters after treatment of psoriasis plaques with calcipotriol the expression of cathelicidin was not decreased but increased . To analyze the effect of vitamin D analogs on cathelicidin expression in vitro a 5 kb fragment of the 5 untranslated region of the human cathelicidin gene CAMP was transfected in keratinocytes and transcriptional activity was assayed. All vitamin D analogs including calcipotriol enhanced cathelicidin promoter activity . Dose- and time-dependent induction of cathelicidin transcript was confirmed in human primary keratinocytes and HaCaT keratinocytes . When used at identical concentrations, calcipotriol exerted similar effects as 1,25D3, the effect of ZK203278 was slightly, the effect of ZK191784 significantly lower and ZK159222 showed the weakest induction of all analogs . Simultaneously, all analogs tested increased the cathelicidin precursor protein hCAP18 in NHEK . Processing of hCAP-18 to active LL-37 peptide could not be detected in our Western blot system.
Vdr And The Mek/erk Signaling Pathway Are Involved In Cathelicidin Induction By Vitamin D Analogs
Having confirmed that vitamin D analogs induce cathelicidin expression underlying signaling pathways were investigated. 1,25D3 increases cathelicidin expression through activation of the vitamin D receptor . To investigate if vitamin D analogs enhance cathelicidin also through the VDR siRNA experiments to silence VDR were performed. Silencing of the VDR significantly reduced the induction of cathelicidin transcript by ZK191784, ZK203278 or calcipotriol . Similarly, Western blot analysis demonstrated silencing of VDR protein expression which resulted in strongly reduced hCAP18 induction after stimulation with vitamin D analogs .
MEK/ERK signaling is critically involved in the regulation of cathelicidin by 1,25D3 in human keratinocytes . To confirm involvement of MEK/ERK signaling in the induction of cathelicidin by vitamin D analogs, primary keratinocytes were transfected with a combination of siRNA oligonucleotides directed against ERK1 and ERK2 . Compared to cells treated with control siRNA silencing of ERK1/ERK2 significantly reduced cathelicidin induction by 1,25D3 and its analogs ZK191784 and calcipotriol. Modest inhibition was observed for induction by ZK203278 .
Read Also: How To Fix Psoriasis On Scalp
Patients And Skin Samples
All treatments and sample acquisitions, including skin biopsies, were approved by the committee on investigations involving human subjects at the Faculty of Medicine, University of Munich, Germany. For all procedures, informed written consent was obtained. Patients did not receive topical treatment before entering the study. 4-mm punch biopsies were taken from a marker psoriatic plaque before treatment with a calcipotriol containing ointment and 5 to 7 days after treatment . Skin biopsies from healthy volunteers served as controls. Additionally, biopsies from untreated lesional and non-lesional skin from psoriasis patients were collected. All biopsies were directly transferred to 1 ml Trizol® or cut and one half transferred to 1 ml Trizol® and the other half to 200 µl RIPA-buffer . All samples were homogenized and mRNA or total protein extraction was performed and analyzed as described below.
Biological Effects Of 1252d And Analogs In Psoriatic Skin
The precise mechanisms underlying the therapeutic effectiveness of vitamin D analogs in psoriasis are still not completely understood. Modulation of various markers of epidermal proliferation and differentiation was shown in situ in lesional psoriatic skin after topical application of vitamin D analogs ., Interestingly, the effects of topical treatment with vitamin D analogs on dermal inflammation are less pronounced as compared to effects on epidermal proliferation or differentiation., This could possibly be explained by the fact that the bioavailability of topically applied vitamin D compounds in the dermal compartment may be markedly reduced as compared to the epidermal compartment.,
In lesional psoriatic skin, the clinical improvement correlates with an increase of VDR mRNA in 1,252D3 treated skin. However, not all patients with psoriasis respond to treatment with vitamin D analogs: responders can be discriminated from non-responders by an increase in VDR mRNA in treated skin areas.
Data concerning serum levels of 1,252D or 25 D in psoriatic patients are also conflicting. Some studies report reduced levels of 1,252D in patients with manifest psoriasis. Additionally, the coincidence of pustular psoriasis with hypocalcemia and the exacerbation of psoriasis along with chloroquin therapy are well known.
Read Also: Best Probiotic Brand For Psoriasis
Are There Side Effects Of Vitamin D
Getting too much vitamin D can have negative side effects. Youre unlikely to get an unsafe amount of the nutrient from food or sunlight. However, you could get too much from supplemental sources.
High levels of vitamin D can cause damage to your kidneys, blood vessels, and heart. In extreme cases, they can cause death. More often, excess vitamin D can lead to high levels of calcium in the blood due to increased calcium absorption. High calcium can cause side effects such as nausea, vomiting, dehydration, confusion, weakness, and kidney stones.
For safety, consult with your health care provider before taking over-the-counter vitamin D supplements. They may check your vitamin D levels, via blood work, prior to recommending a supplement.
Vitamin D And Psoriasis Linkage
In psoriasis, vitamin D is involved in the maintenance of cutaneous barrier homeostasis. Several studies identified an association between polymorphisms of vitamin D receptor and psoriasis susceptibility . Richetta et al., have found that the A-1012G promoter polymorphism of the VDR gene is associated with psoriasis risk through a lower expression of VDR mRNA, favoring conditions that may alter cutaneous barrier and the development of psoriatic lesions . In addition, in psoriatic skin a decreased expression of VDR and reduced tight-junction proteins is associated . Tight junctions are fundamental to regulate adhesion and permeability of keratinocytes, and to polarize cutaneous cell differentiation, to regulate extracellular calcium gradient, interacting with nuclear and cytoplasmic proteins and influencing the regulation of specific genes involved in keratinocytes differentiation and proliferation . Different studies have focused on the possible role of low vitamin D status in the pathogenesis of psoriasis .
You May Like: Best Coconut Oil For Psoriasis
Risks And Shortcomings Of Vitamin D
Vitamin D can help many people with psoriasis. Still, its often not an effective long-term treatment on its own. Some people will need topical medications with other active ingredients, including corticosteroids. Vitamin D also wont work for everyone, regardless of what form its taken in.
The biggest risk of taking vitamin D is taking too much. Vitamin D in moderation is good for you, but taking too much can hurt you. It causes a condition called hypervitaminosis D, or vitamin D toxicity. This condition can cause a buildup of too much calcium in the blood, which can cause frequent urination, weakness, and eventually kidney problems. Its typically only caused by excessive doses of vitamin D supplements. It almost never occurs from diet or sunlight exposure.
As long as you take vitamin D in moderation, you should be able to avoid vitamin D toxicity. Your risk increases, though, if you have liver or kidney conditions already.
The Nutritionist And Vitamin D Supplementations
Supplements are the most important determinant of variation in vitamin D intake A number of studies showed that the daily intake of vitamin D was higher in adults using vitamin D supplements than in those without vitamin D supplementations . Most nutritionists recommend the use of vitamin D3 to treat and prevent vitamin D deficiency, because several studies indicating a higher efficacy for vitamin D3 in raising serum 25D concentrations when compared to vitamin D2 . Although a significant inter-individual variation exists, due to different variables including body weight, sunlight exposure and calcium intake, it has been calculated that supplementation of 1000 IU of vitamin D3 daily leads to an approximate increase in 25D levels by 1020 ng/mL , . Findings from randomised placebo-controlled trials conducted during the winter have shown that each 1 mg of supplemental vitamin D is associated with an increase in serum 25D of between 0.7 nmol/L and 2 nmol/L .
Also Check: Best Treatment For Psoriasis And Psoriatic Arthritis
Changes In Antimicrobial Peptide And Inflammatory Cytokine Expression In Psoriatic Plaques After Treatment With Calcipotriol
4-mm punch biopsies from a marker psoriatic plaque were taken from patients before and after treatment with ointment containing the vitamin D analog calcipotriol . Total mRNA was extracted and transcript levels of cathelicidin, HBD2, HBD3, psoriasin, IL-17A, IL-17F and IL-8 were analyzed by qPCR. Expression of antimicrobial peptides and markers of inflammation in untreated, lesional skin of psoriasis patients was normalized to the mean expression of target genes in skin of the healthy controls . In the relative changes of gene expression levels in calcipotriol treated vs. untreated lesional skin of psoriasis patients are displayed. The Y-axis in and is depicted in Log10 scale . Punch biopsies from lesional and non-lesional psoriatic plaque were taken from patients . Total mRNA was extracted and transcript levels of cathelicidin and HBD2 analyzed by qPCR. Statistical analysis of lesional or non-lesional, respectively, psoriatic skin vs. healthy controls was performed with Mann-Whitney test, comparison of lesional vs. non-lesional biopsies was performed with Wilcoxon matched pairs test . In Western blot analysis using an antibody which detects HBD2 was performed with total protein extracted from biopsies taken from lesional skin of one representative psoriasis patient before and after treatment with calcipotriol.
Why Dermatologists Prescribe Synthetic Vitamin D To Treat Psoriasis
Synthetic vitamin D can:
-
Slow rapidly growing skin cells
-
Flatten thick psoriasis
-
Synthetic vitamin D is considered safe for most patients, including children
-
It clears psoriasis in some patients, including patients who have scalp psoriasis
-
Most people notice an improvement after using it for two weeks
-
If a patient needs stronger medicine, synthetic vitamin D can be safely combined with a strong corticosteroid
Studies show that using both tends to be more effective than using either medication alone.
-
Using both synthetic vitamin D and a corticosteroid can also reduce the possible side effects that come with using a strong corticosteroid
-
The combination can be used for much longer than a strong corticosteroid alone
Recommended Reading: What Is Good For Psoriasis
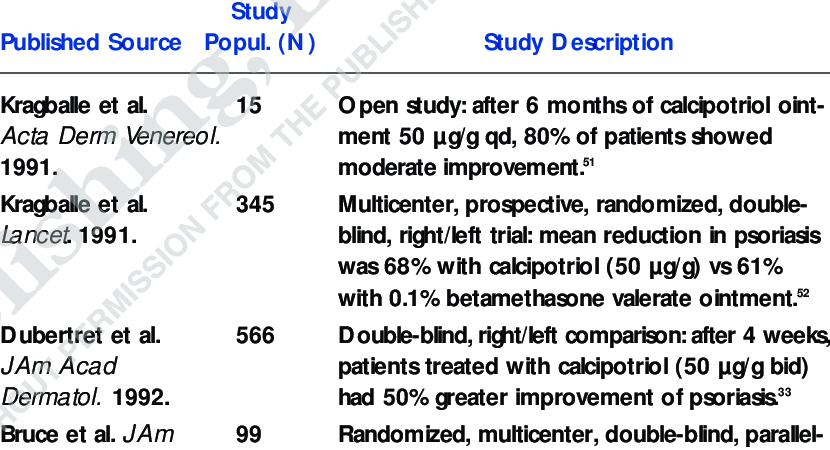
Monotherapy With Vitamin D3 Analogues For Long
The first open pilot study on topical long-term use of calcipotriol 50 g/g was conducted in 1991 by Kragballe et al. in 15 patients with psoriasis vulgaris for six months . At the end of the study 80% had shown an at least moderate response to the treatment with an overall good tolerability. A number of non-randomized open observational studies followed for calcipotriol 50 g/g , , , , , calcitriol 3 g/g – and tacalcitol 420 g/g , -. The most impressive therapeutic results of topical treatment with vitamin D3 analogues usually became evident during the first 4 weeks after treatment was initiated , . Later on improvement of the skin condition was only moderate. In blinded trials, a 4-week induction therapy with a fixed combination of calcipotriol 50 g/g with betamethasone dipropionate 0.5 mg/g followed by a maintenance monotherapy with calcipotriol 50 g/g yielded an at least satisfactory therapeutic result in 56 % to 58 % of the patients after 52 weeks . In open observational studies , adjusted response rates were higher: 78 % to 80 % with calcipotriol, while a standard regimen of tacalcitol led to an adjusted response rate of 5659 % , , increasing to 69 % at higher dosages . For calcitriol 3 g/g, the adjusted response rate was 40 % -.
Vitamin D For Psoriasis: Benefits And Uses
Increasing your vitamin D intake can be a valuable step toward controlling your psoriasis symptoms. The nutrient can be obtained naturally from certain foods and from sunlight exposure, as well as from oral supplements and creams. Vitamin D is best known for its role in calcium absorption, which is vital for bone and teeth health. However, its also important for supporting the health of other systems notably, the immune system and skin.
If you have psoriasis, you know that its caused by an overactive immune response that leads to inflammation and itchy skin buildup. Treatments for psoriasis work by targeting the immune systems response or by helping to relieve symptoms.
Recommended Reading: How Fast Does Psoriasis Spread
Vitamin D Analogs Block Il
The understanding of the crucial role of IL-17A in skin inflammation in psoriasis is rapidly evolving . Among its multiple activities IL-17A was recently identified as a very potent inducer of HBD2 . HBD2 belongs to the -defensin family and the -defensins have been directly linked to psoriasis pathogenesis . Therefore the effect of the vitamin D analogs calcipotriol and ZK191784 on IL-17A induced HBD2 expression was analyzed in keratinocytes in vitro. IL-17A strongly induced HBD2 transcript abundance in NHEK and induction was significantly reduced by calcipotriol and ZK191784 . A dose-dependent inhibition of HBD2 induction was confirmed with increasing concentrations of calcipotriol . At the same time the induction of IL-8 by IL-17A was decreased by calcipotriol .