When Does Psoriatic Arthritis Develop
Psoriasis and psoriatic arthritis can appear at any age. Psoriasis often has two stages where onset is most common. The first is between the ages of 20 and 30, and the second is between the ages of 50 and 60.
Psoriatic arthritis most commonly develops between the ages of 30 and 50.
Quality Of Life And Psychological Aspects Of Psoriasis
Although psoriasis generally does not affect survival, it certainly has a number of major negative effects on patients, demonstrable by a significant detriment to quality of life. Despite this, most clinical trials of new treatments for psoriasis focus on objective physical measures for the primary endpoint of efficacy. This is incongruous as it is the improvement in quality of life that patients and physicians rely upon when selecting treatment. Impairment of quality of life has been highlighted particularly by the work of Finlay. Patients with psoriasis have a reduction in their quality of life similar to or worse than patients with other chronic diseases, such as ischaemic heart disease and diabetes. That patients with psoriasis feel stigmatised by the condition is well established. This of itself contributes to everyday disability leading to depression and suicidal ideation in more than 5% of patients.
Furthermore, quality of life measures take into account the effect of the treatment on the patient. Quality of life data fulfils the role of measuring the intangible changes in a patients life that determine treatment success. For a clinically meaningful change to exist for psoriasis and other chronic, non-life threatening diseases, a treatment must provide an improvement in the patients quality of life. In an attempt to provide an holistic assessment of overall disease severity, a specific tool has been developedthe Salford Psoriasis Index :
The Link Between Psoriasis And The Immune System
No one ever really considered that the immune system had any real role in psoriasis, or its painful outbreaks. Not until a new drug Cyclosporine was offered to arthritis patients. What happened next was both surprising and unexpected. Patients who were prescribed the immune suppressing drug for their arthritis symptoms , began to report a decrease in their skin attacks. Without warning, researchers were faced with the theory that the immune system could be causing psoriasis.
It didnt take long before researchers began to figure out the mystery of psoriasis in regards to how the immune system can impact it.
The Role of the Immune System on the Skin
The immune system is responsible for standing guard and attacking any invaders which penetrate the body. Since the skins main job is to act as the bodys first defense mechanism against invasion, it is no wonder that the immune system works in close connection with each layer of the skin. Heres how it all works:
1. Immune cells patrol the entire body for dangers. Percent of Population With Psoriasis
2. When an invader is detected, these immune send out chemical and nervous system messages to the immune system to ready itself for an attack
Don’t Miss: List Of Biologics For Psoriasis
Reasons For Discontinuing Treatment
Providers documented the reasons for treatment discontinuation after conversations with the patient. The providers selected from loss of efficacy, side effects, inability to comply with treatment regimen, inability to afford treatment, patient fear or risk, or unknown. Providers could select more than one reason.
Healthcare resource utilization
Visit frequency was defined as the number of patient visits during the study period.
What Is Plaque Psoriasis
Plaque psoriasis, which is recognizable due to the scaly plaques it produces on the skin, is the most common type of psoriasis. An estimated 80 to 90 percent of people with psoriasis develop plaques.
Some people will have more than one type of psoriasis. People who have plaque psoriasis may later develop other forms of the condition, such as psoriatic arthritis.
Usually, the turnover of peoples skin cells takes 21 to 28 days. In people with psoriasis, the body attacks healthy skin cells, so new cells develop every 4 to 7 days.
Psoriasis damages patches of skin, leaving areas of redness and irritation. This damage causes the skin to appear scaly and gray and to peel off.
Plaque psoriasis is not an infection, and it is not contagious. However, irritated patches of psoriasis can become infected.
In some people, an infection or injury to the skin can trigger an outbreak of psoriasis. People experiencing their first psoriasis flare-up may mistake their symptoms for an allergic reaction or skin infection.
Read Also: Where Does Psoriasis Come From
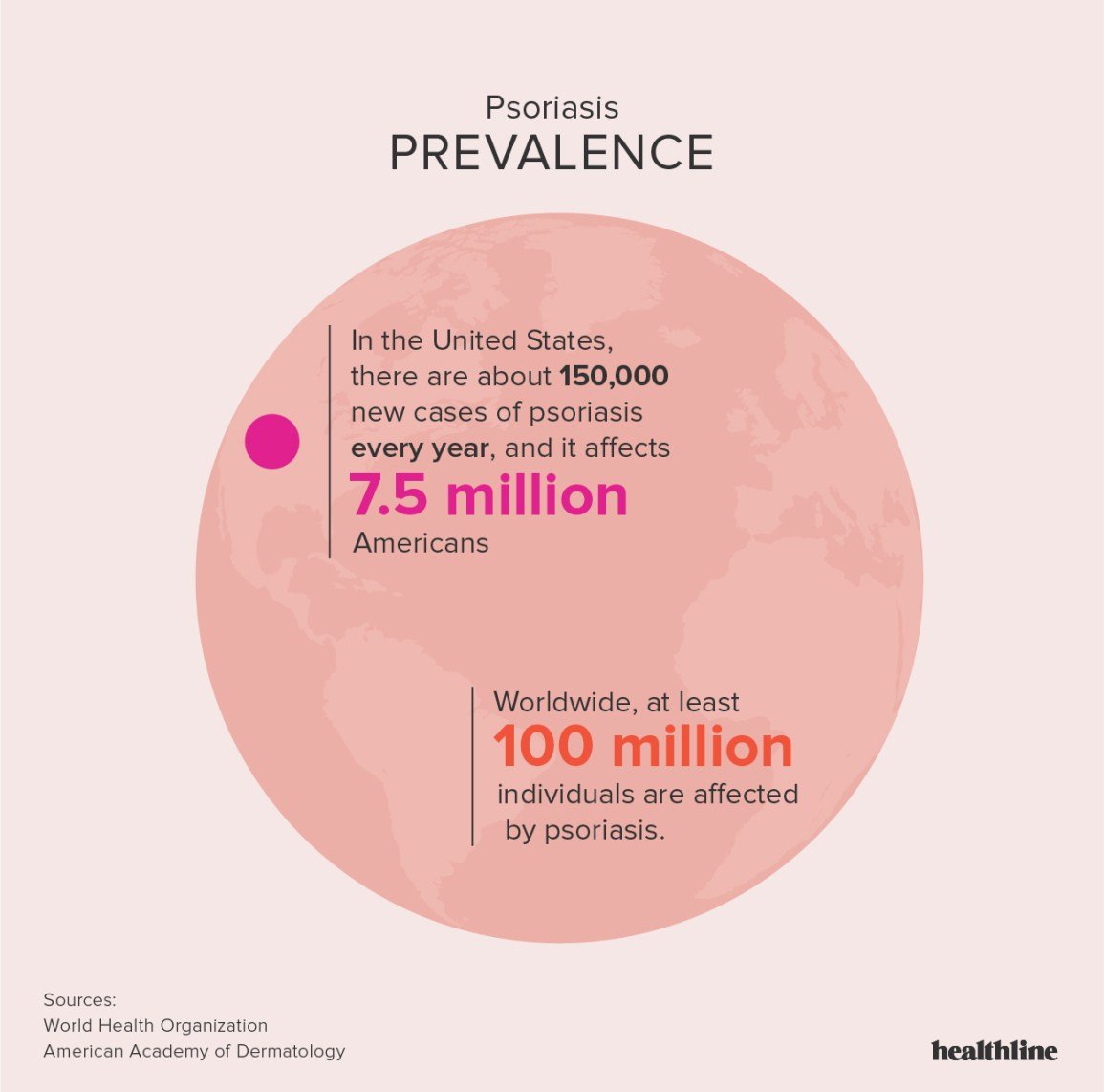
How Common Is Psoriasis
Although it is difficult to estimate exactly how many people are living with psoriasis, it is thought that the disease affects at least 125 million people around the world. This means that about 2 percent to 3 percent of the global population have some form of psoriasis.1,2
Surveys suggest that around 3 percent of all people over age 20 living in the U.S. have been diagnosed with psoriasis, or 7 million adults.-3
However, researchers think that it is likely that many more than 7 million people in the United States have the disease. This is because many people may not have been diagnosed by a healthcare provider yet, or do not know for sure that they have psoriasis.3
Some Symptoms Associated Psoriatic Arthritis
Symptoms can vary greatly from patient to patient. Let your doctor know if you have the following symptoms which may indicate psoriatic arthritis:
- Joint pain especially with redness, swelling and tenderness.
- Dactylitis inflammation of an entire digit, either a finger or toe which swells up to a sausage shape and can be painful.
- Nail changes loosened, thickened or pitted nails .
It has been suggested that the presence of 20 nail pits distinguishes patients with PsA from those with rheumatoid arthritis and psoriasis.
- Morning stiffness/pain in the back that improves with movement.
- Pain in your heel or tennis elbow.
Read Also: Over The Counter Psoriasis Treatment At Walmart
How Is Psoriasis Diagnosed
Psoriasis is generally diagnosed by a physical examination of the skin, as well as a medical and family history. The doctor may also take a biopsy to examine under a microscope. While a general practitioner may diagnose psoriasis, people with skin conditions may wish to consult with a dermatologist, a specialist on skin disorders.2
Read Also: What Kind Of Doctor Treats Psoriasis
Protection Of Human Subjects
This study was approved by the University of Pennsylvania Institutional Review Board and CMS . Per CMS Data Use Agreement, any data cells containing fewer than 11 beneficiaries were not shown. The study was conducted in accordance with the Declaration of Helsinki and reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Don’t Miss: How To Prevent Guttate Psoriasis
How Is Psoriasis Diagnosed And Treated
Psoriasis often has a typical appearance that a primary care doctor can recognize, but it can be confused with other skin diseases , so a dermatologist is often the best doctor to diagnose it. The treatment of psoriasis usually depends on how much skin is affected, how bad the disease is , or the location . Treatments range from creams and ointments applied to the affected areas to ultraviolet light therapy to drugs . Many people who have psoriasis also have serious health conditions such as diabetes, heart disease, and depression. Some people with psoriasis also have an inflammatory condition which affects their joints, called psoriatic arthritis.
Psoriatic arthritis has many of the same symptoms as other types of arthritis, so a rheumatologist is often the best doctor to diagnose it. The treatment of psoriatic arthritis usually involves the use of drugs .
Psoriatic disease may be treated with drugs or a combination of drugs and creams or ointments.
Psoriatic Arthritis By The Numbers
Psoriatic arthritis question and answer:
How many people have psoriatic arthritis? In the United States psoriasis occurs in about 2% of the population and equally among the sexes. In people diagnosed with psoriasis, about 5%to10% will go on to develop psoriatic arthritis.
When do individuals first begin noticing symptoms? Around 85% of individuals living with psoriatic arthritis have lived with psoriasis for years prior to the onset of arthritis. Symptoms of psoriatic arthritis typically occur between ages 30 and 50, with most cases starting between the fourth and fifth decade.
Does everyone with psoriasis get psoriatic arthritis? No. Studies have shown that anywhere from 5% to 30% of individuals living with psoriasis will go on to develop psoriatic arthritis. This wide discrepancy in incidence is due to variations in definitions and design from one clinical trial to another over time.
Are there different types of psoriatic arthritis? There are five types of psoriatic arthritis: symmetric , asymmetric , distal interphalangeal , spondylitis , and arthritis mutilans .
How many people are severely affected by psoriatic arthritis? About 20% of individuals living with psoriatic arthritis are characterized as suffering from severe psoriatic arthritis affecting four or more joints.
Recommended Reading: Is Lubriderm Good For Psoriasis
How Many People With Psoriasis Develop Psoriatic Arthritis
About one in three people with psoriasis will develop psoriatic arthritis. About 85% of people with psoriatic arthritis develop psoriasis first.
Typically, psoriatic arthritis occurs between the ages of 30 and 50, but it can occur at any time.
In many people, psoriatic arthritis develops about 10 years after the onset of psoriasis.
Strengths And Limitation Of The Study

The study has several key strengths. Firstly, we undertook an extensive systematic review to search for all available literature since inception by using 11 electronic and regional databases with no restriction on language. Secondly, we used a bayesian framework approach to analyse the data, which is the optimal technique when data are sparse and heterogeneous. Thirdly, the statistical model was adjusted for potential sources of heterogeneity, such as age strata, type of diagnostic method, and type of prevalence measure used to calculate the prevalence of the disease. Finally, our analysis generated estimates for 21 regions and 189 countries of the world.
Don’t Miss: Can You Develop Psoriasis In Your 60s
Overview Of The Methodology
This study is part of the GBD 2019 , which, to the best of our knowledge, is the most comprehensive, methodologically robust report to date, which systematically estimates the spatial levels and temporal trends of the global burden caused by 369 diseases and injuries, as well as by 87 risk factors, in the period from 1990 to 2019. Seven super-regions, 21 regions, and 204 countries and territories were involved in the GBD 2019. The GBD 2019 adopts a 4-level hierarchical framework to classify and list causes as aggregate groupings. While level 1 causes include non-communicable disorders, injuries, and a category combining infectious, maternal, neonatal, and nutritional diseases/impairments, level 2 lists 22 diseases and injuries such as respiratory infections, cardiovascular disorders, and transport injuries. Level 3 and level 4 causes include specific causes, which differ based on the amount of details provided. For instance, psoriasis is a level 3 cause. Detailed GBD methodology is published elsewhere .
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
You May Like: Cerave Psoriasis Moisturizing Cream Cvs
Up To 30 Percent Of People With Psoriasis Will Go On To Develop Psa And 85 Percent Of People With Psa Also Have Skin Psoriasis
Psoriasis and psoriatic arthritis are distinct conditions, but they are connected. In fact, data show that up to 30 percent of people with psoriasis will go on to develop PsA and 85 percent of people with PsA also have skin psoriasis.
Although people can be diagnosed with PsA without having any skin involvement, most often they will have a family member with skin psoriasis, says Rebecca Haberman, MD, a rheumatologist at NYU Langone Health in New York City.
Psoriasis is an inflammatory condition of the skin, while psoriatic arthritis also includes inflammation of the joints and entheses , .
Read on to find out the different symptoms of psoriasis vs. PsA, how they are diagnosed and treated, and what you need know about the link between these health conditions.
Are Some People More Likely Than Others To Develop Psoriasis
People of all ages can develop psoriasis. About one-third of people with psoriasis are diagnosed with the disease before the age of 20, and around three-quarters of people are diagnosed before the age of 40. Some people who have never had the condition before will develop it for the first time between the ages of 50 and 60.1,3
Psoriasis affects men and women at equal rates.3
About one-third of people with psoriasis report having a relative with the condition. If a parent has psoriasis, their child has about a 10 percent chance of developing it too. If both parents have psoriasis, their child has about a 50 percent chance of developing the disease.2 Incident rates in children have more than doubled since 1970. Children also are more likely to have serious co-occurring health issues such as depression, anxiety, obesity, diabetes, high blood pressure, high cholesterol, and rheumatoid arthritis.4
Psoriasis can affect people of all ethnicities. In the U.S., research has shown that psoriasis is more common among people of certain ethnicities than others. For example, researchers estimate that in the United States, around 2.5 percent of non-Hispanic Caucasians have psoriasis compared to 1.3% of African Americans. About 80 percent, reported mild disease.1,3
People with psoriasis report more mental distress or mild to severe depression than those without psoriasis. They are also more likely to be obese and be a former smoker.3
Also Check: Best Cream Psoriasis Over Counter
What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
You Might Hear: Whats The Big Deal Its Just A Rash
Yes, psoriasis can be itchy and aggravating. But what many people dontrealize is that its a serious health condition.
âIm sometimes surprised when people act like its just psoriasis,’ says Gary Spivak, who also has the common disorder. âIt can lead to skin infections and scarring, and research even shows that its linked to an increased risk of heart problems.â
What you can do:
You dont have to explain the seriousness to everyone. But if a friend, family member, or colleague asks, you could look at it as an opportunity to spread awareness, Jacob says.
Ineson also approaches it as a teaching moment. And a little humor never hurts. âIf that was the case, Iâd be lathered in cream,â she says.
Don’t Miss: Does Psoriasis Affect Your Nails
Comparison With Other Studies
Research performing similar analyses is limited. Hay and colleagues provided estimates of the prevalence of psoriasis for 21 regions of the world. Our estimates are lower than their findings, with the main differences in the data sources used. Our systematic review was more extensive and included more recent studies. Furthermore, our statistical model adjusted for important sources of heterogeneity, such as type of diagnostic methods and type of prevalence measure. If we restricted our analysis to the self-reported lifetime prevalence of psoriasis, our estimate of the global prevalence of psoriasis would be similar. A major strength of our research compared with Hay and colleagues and James and colleagues is that we were able to provide a measure of the prevalence of psoriasis for 189 countries. Importantly, data included in our study cover the most comprehensive existing scientific literature identified from 11 electronic and regional databases compared with two electronic databases searched in the studies by Hay and colleagues and James and colleagues.