When Can You Get A Covid
It will be up to your states guidelines. The NPF notes that, as a psoriatic disease patient, you may be in a high-priority group for vaccination if you have psoriasis-associated comorbidities. These may include those known to increase COVID-19 risk or those that might increase COVID-19 risk .
You may also be prioritized if you take medications classified by the CDC as lowering your bodys ability to fight some infections, such as corticosteroids.
Either way, you likely dont need to wait long: The White House recently declared that all adults in the United States will be eligible for vaccination no later than May 1.
To help ensure every adult will have access to the vaccine by May 1, government officials are increasing the number of locations where people can get vaccinated , expanding the professionals who can administer shots , and providing tools to make it easier to find vaccines , per The White House.
I encourage all my psoriatic arthritis patients to get the COVID-19 vaccine as soon it is available to them, says Dr. Gupta. Patients should take the first COVID-19 vaccine any of those currently approved for which they are eligible and offered based on federal, state, and local guidance.
Once you get your vaccine, you still need to be careful to follow standard mitigation efforts. For more information, heres what immunocompromised people should know about the CDC recommendations for fully vaccinated people.
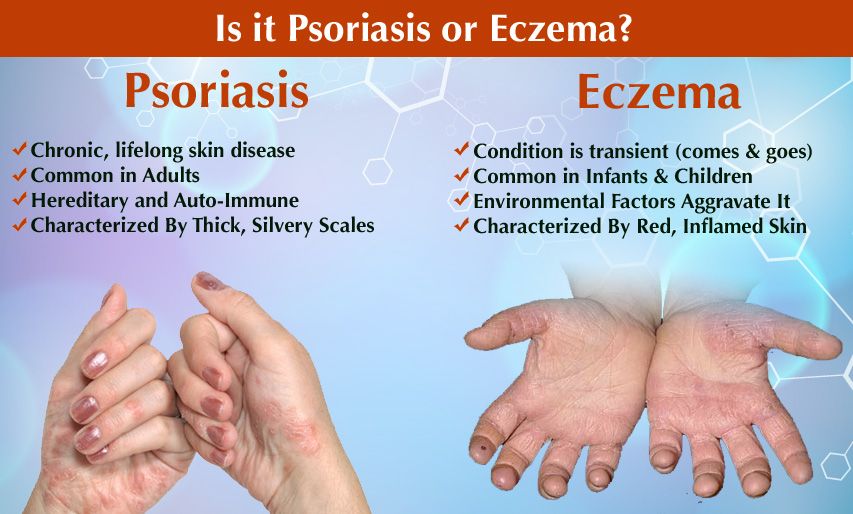
Is Psoriasis The Same As Eczema
Psoriasis and eczema are two different skin conditions. They differ in where the disease appears on the body, how much it itches and how it looks. Eczema tends to appear more often behind the knees and inside the elbows. Eczema also causes more intense itching than psoriasis. Many people, especially children, can get both eczema and psoriasis.
What Is Plaque Psoriasis
Plaque psoriasis is the commonest form of psoriasis which is characterized by the appearance of reddish well-demarcated plaques with silver scales usually on the extensor surface of the knees and elbows. Lower back, scalp, and ears are the other common sites affected by this condition. New plaques can emerge at the sites of new trauma. This is known as the Kbner phenomenon. Occasionally the lesions can become itchy or sore.
Figure 02: Plaque Psoriasis
Plaque psoriasis is managed in the same manner as mentioned above.
Read Also: Types Of Biologics For Psoriasis
Who Can Take Biosimilars
All biologics, including biosmilars, are typically prescribed for people with more advanced disease, including individuals with moderate-to-severe psoriasis and active PsA. But each of the three approved biosimilars are indicated for different groups within this population.
You should not take biosimilars if:
- Your immune system is significantly compromised
- You have an active infection
Screening for tuberculosis or other infectious diseases is required before starting treatment with all biologics, including biosimilars.
What Else Should I Ask My Healthcare Provider

If you have psoriasis, ask your healthcare provider:
- How can I prevent outbreaks and control symptoms?
- What medication will work best for me?
- What else should I do to improve symptoms?
- What are my options if creams dont work?
- Will psoriasis ever go away?
A note from Cleveland Clinic
Psoriasis, an itchy skin condition, can come and go throughout your life. Its related to an overactive immune response and is not contagious. If you have skin changes that arent going away, talk to your healthcare provider. There is no cure for psoriasis, but psoriasis treatments can improve symptoms. Your provider may prescribe a special cream or moisturizer or medications. Other therapies are available if creams or medicines dont work. Maintaining your overall health will also help improve symptoms.
Last reviewed by a Cleveland Clinic medical professional on 10/17/2020.
References
Also Check: Home Remedies For Itchy Scalp Psoriasis
What Is Difference Between Psoriasis And Psoriatic Arthritis
24.08.2020.
How is it different than eczema? · Eczema is much more commonly found in children · It is rare for someone to have both eczema as a child and.
Facts about Psoriatic Arthritis 1. Psoriatic arthritis is a type of arthritis that occurs along with psoriasis in an estimated 10-30 percent of cases. Psoriasis is a skin condition that causes patches of skin to become red and scaly. 2. Psoriatic arthritis usually develops after skin symptoms, but it is possible for symptoms of arthritis to.
01.06.2020.
in the treatment of psoriasis and psoriatic arthritis .
The RESPOND study, an open-label comparison of MTX and infliximab,
Psoriatic Arthritis Vs. Rheumatoid Arthritis: How the 2 Conditions Differ, According to Experts Heres what you need to know about the similarities and differences between these two rheumatic.
is a good amount of overlap. Video: Psoriatic Arthritis Vs. Rheumatoid Arthritis: How the.
However, distinct immunopathogenic, phenotypic and genetic differences exist between these two.
for Research and Assessment of Psoriasis and Psoriatic Arthritis has been instrumental in.
Under this hypothesis, psoriasis without arthritis was not a risk factor.
that professionals in the field may have different opinions.
The exact relationship between psoriatic arthritis and.
s site is chock-full of information about psoriasis and psoriatic arthritis. You can request a free electronic psoriatic arthritis.
01.05.2013.
16.09.2014.
28.07.2021.
24.05.2021.
You Can Develop Psoriatic Arthritisanytimebefore Or After Your Psoriasis Diagnosis
Medical experts used to believe that people with psoriasis could only develop psoriatic arthritis within 10 years of their initial psoriasis diagnosis, according to the Cleveland Clinic. However, studies have shown that this isnt true. In fact, up to 15% of people with both diseases actually experienced their psoriatic arthritis symptoms first, according to the Cleveland Clinic. Some people may develop psoriatic arthritis before psoriasis, and others may have had psoriasis for years without realizing it, according to Dr. Giangreco. Psoriasis can remain hidden from patients on the back of the scalp or buttock area and go unnoticed for long periods of time, Dr. Giangreco tells SELF. If you have psoriatic arthritis and suddenly notice changes in your skin and nails, then you dont want to rule out the possibility of psoriasis. Rarely do people have psoriatic arthritis without getting psoriasis, too, according to the U.S. National Library of Medicine.
Also Check: What Are Symptoms Of Plaque Psoriasis
Link Between Psoriasis And Inflammatory Bowel Disease
What is inflammatory bowel disease? IBD can include Crohns disease and ulcerative colitis. Learn more about testing, treatments, and the home care needed to manage IBD. home digestive disorders center digestive disorders a-z list slideshow.
Rationale and background: Inflammatory bowel disease has been reported to frequently co-occur in patients with manifest psoriasis and psoriatic.
Epidermolysis bullosa acquisita and inflammatory bowel disease. JAMA 1983 250:1746. Najarian DJ, Gottlieb AB. Connections between psoriasis and.
To evaluate the association of psoriasis and PsA with IBD and other GI illnesses, the researchers identified data from the National.
Psoriasis and the spectrum of inflammatory bowel diseases are chronic, inflammatory, organotropic conditions. The epidemiologic coexistence of these diseases is corroborated by findings at.
Results: Prevalence of inflammatory bowel disease, Crohn’s disease and ulcerative colitis in patients with psoriasis vs the general population in 2011 were 0.16, 0.05 and 0.12% vs 0.08, 0.03 and 0.
Psoriasis and the spectrum of inflammatory bowel diseases are chronic, inflammatory, organotropic conditions. The epidemiologic coexistence of these diseases is corroborated by findings at.
Background: The epidemiology of the association between psoriasis and inflammatory bowel disease is poorly defined and remains controversial.
studies showing there may be equipoise between chemoradiation and surgery and chemo.
Psoriasis And Psoriatic Arthritis Can Severely Affect Your Quality Of Life
People with either condition frequently say that their health informs their decision-making, from the clothes they buy to their careers. Thats because both conditions can drastically change your life, making it difficult to sleep, work, and do the things you love, like playing with your children or baking. For example, when you have a psoriasis flare, even rolling over in bed or wearing tight clothing can be extremely painful. Some people with psoriasis choose clothing that hides their flares to avoid getting comments about their skins appearance. Similarly, joint pain from psoriatic arthritis can make it really hard to sit on the floor with your kids, get out of bed for work, or follow through on plans. This can all become overwhelming, and understandably make some people feel self-conscious about their health conditions.
Recommended Reading: Is Psoriasis A Serious Disease
Are Treatment Plans All That Different
Despite presenting very differently, there are many of the same treatment options for PsO and PsA, including nonsteroidal anti-inflammatory drugs and biologic drugs like Enbrel , Cosentyx , and Humira . There are, however, a few variances. For instance, as Dr. Friedman explains, unlike psoriasis, psoriatic arthritis typically doesnt respond to topical creams, as it primarily affects the joints, and creams are unable to effectively penetrate the dermis and reach the nerves underneath.
PsA needs to be treated with systemic therapies, such as biologics, for which we have many, Dr. Friedman says. But there are a good number of treatments approved for both plaque psoriasis and psoriatic arthritis. Biologic drugs, for example, work for both PsA and PsO by blocking certain cells or proteins in our immune systemsuch as the T-cell or the tumor necrosis factor-alpha proteinthat largely contribute to the development of psoriasis and psoriatic arthritis.
Dr. Finney adds that because joint changes associated with PsA can be permanent, prompt systemic treatment is highly warranted if someone does notice joint symptoms. Below, find a few systemic treatments for PsA and how they work.
Can Biosimilars Be Used With Other Treatments
It is important to tell your health care provider about all treatments, medicines, vitamins or supplements that you are taking.
Like all biologics, biosimilars can be used with other treatment options including topicals and phototherapy. The biologics Enbrel, Humira and Remicade are shown to be safe and effective when taken with methotrexate. This means that their biosimilars, including Erelzi, Amjevita, and Inflectra, may be safe and effective when taken with methotrexate.
- With Inflectra being the biosimilar to Remicade, its use in combination with phototherapy may increase the risk for skin cancer.
- No drugs that interact with biologics should be combined with their respective biosimilars.
Don’t Miss: What Is The Reason For Psoriasis
Are There Complications Of Psoriasis
In some people, psoriasis causes more than itchiness and red skin. It can lead to swollen joints and arthritis. If you have psoriasis, you may be at higher risk of:
- Use medicated shampoo for scales on your scalp.
Other steps you should take to stay as healthy as possible:
- Talk to your healthcare provider about lowering your risk for related conditions, such as heart disease, depression and diabetes.
- Lower your stress with meditation, exercise or seeing a mental health professional.
What Are The Types Of Psoriasis
Chronic plaque psoriasis: Raised, red, scaly patches mainly occurring on the limbs and the trunk, especially on the elbows, knees, hands, around the navel, over the lower back and on the scalp. The nails may be affected so that they become thickened and raised from their nail beds, and the surface of the nail may be marked with small indentations . This is the most common type of psoriasis, affecting approximately 9 out of 10 people with psoriasis.
Guttate psoriasis : So named because it manifests itself over the body in the form of scaly, droplet-like patches. Numerous small, red, scaly patches quickly develop over a wide area of skin, although the palms and the soles are usually not affected. It occurs most frequently in children and teenagers, often after a throat infection due to streptococcal bacteria. Some people who have had guttate psoriasis will go on in later life to develop chronic plaque psoriasis.
Scalp psoriasis: Raised, red, thick, scaly plaques on the scalp and around the hairline. It is common and approximately 1 out of 2 of all people with psoriasis have it on their scalp. The reason it deserves special mention is that it can be particularly difficult to treat and usually requires specifically formulated medicines. It is awkward to treat with creams and ointments because the hair gets in the way. See Scalp psoriasis for more information
Recommended Reading: What Soap Is Best For Psoriasis
Are People With Psoriatic Arthritis At Greater Risk For Covid
This is an ongoing area of research.
The National Psoriasis Foundations guidance says that it is not known with certainty if having psoriatic disease meaningfully alters the risks of contracting SARS-CoV-2 or having a worse course of COVID-19 illness. It notes that existing data, with some exceptions, generally suggest that patients with psoriasis and/or psoriatic arthritis have similar rates of SARS-CoV-2 infection and COVID-19 outcomes as the general population.
The ACRs guidance says that autoimmune and inflammatory rheumatic disease patients are at higher risk for being hospitalized due to COVID-19 and having worse outcomes compared to the general population.
However, this is likely affected by factors such as age, other comorbidities such as heart disease or obesity, which is common in PsA, and taking steroid medications, rather than simply having psoriatic arthritis alone.
Some data suggests that patients with inflammatory rheumatologic diseases who get COVID-19 may have higher risk of developing serious complications, depending on their disease activity and other medical conditions such as high blood pressure, diabetes, and chronic kidney and lung disease, adds Dr. Zhu.
For more information, check out this summary of research on inflammatory arthritis and rheumatic disease patients and their risk for COVID-19 complications.
How Are Psoriasis And Psoriatic Arthritis Connected
You may have heard that psoriatic arthritis and psoriasis are connected, but might not understand how. Although the conditions share a similar name, they can have some very different symptoms and treatments. People with psoriasis are at a greater risk of developing psoriatic arthritis, and sometimes people with psoriatic arthritis develop psoriasis later on, meaning its helpful to have an understanding of both conditions if you are diagnosed with one, according to the Mayo Clinic.
Untangling the nuances between these two conditions can be a bit complicated. Thats why we spoke with experts about the important things you should know about psoriatic arthritis and psoriasis, including how the two are linked.
Also Check: How To Reduce Redness In Psoriasis
Articles On Psoriasis Symptoms
Maybe you’re settling into your easy chair for a little Sunday siesta. Or you’re heading out the door for a day of fun in the sun. Either way, you stop and pause, because you’ve got an itch that just won’t leave you alone — along with blotches of red on your skin. What gives?
Your doctor needs to make the final call, but psoriasis or eczema could be the problem. Both are skin conditions with similar symptoms, but there are ways to tell them apart.
What Is The Difference Between Plaque Psoriasis And Psoriatic Arthritis
Psoriasis is an autoimmune disorder that manifests as a chronic skin condition. Psoriasis can lead to the development of plaques, which are patches of scaly, red or white skin. Many individuals with psoriasis are later diagnosed with psoriatic arthritis, which is a condition with similar causes that results in joint pain, stiffness and swelling..
Both plaque psoriasis and psoriatic arthritis develop as a result of an autoimmune disorder, which is when the immune system attacks the body, leading to inflammation and/or pain. While psoriasis and skin symptoms typically develop before psoriatic arthritis, there are some cases in which arthritis develops months or even years before skin symptoms appear. In addition to a link to the immune system, doctors believe there is a link between more severe cases of psoriasis and the development of psoriatic arthritis. Additionally, many people with psoriatic arthritis have a parent or sibling with the disease. It most commonly occurs in adults between the ages of 30 and 50.
Read Also: Best Over The Counter Shampoo For Psoriasis
Why Some People With Psoriasis Develop Psa
Although psoriasis and PsA may appear unrelated, both conditions reflect underlying immune system problems.
In psoriasis, your overactive immune system causes your bodys skin cells to develop too rapidly. This can be triggered by many environmental factors, such as stress or smoking.
One thing these triggers have in common is that they stimulate your bodys inflammation response. This same inflammation response can happen in your joints. Inflamed joints are what cause PsA.
In PsA, white blood cells target your bodys tissues instead of protecting your body against foreign substances. Though PsA is connected to psoriasis, it has very distinctive symptoms of its own. For this reason, some researchers have referred to PsA as a disease within a disease.
The Centers for Disease Control and Prevention calculates that 10 to 20 percent of people with psoriasis will go on to develop PsA. This is slightly lower than the figures provided by the National Psoriasis Foundation, which put the risk at about 1 in 3, or 30 percent.
Psoriasis is typically diagnosed by the onset of plaques. These are scaly patches of raised, silver-white or reddish skin. PsA affects your joints, typically those in your fingers, toes, and lower back.
PsA can come in many forms. It can trigger other side effects such as fatigue and decreased range of motion. Because psoriasis is more visibly apparent, its often easier to diagnosis than PsA.
Psoriatic Arthritis: What Is The Connection
Psoriatic arthritis : 1 in 4 of people with psoriasis may develop an associated arthritis called psoriatic arthropathy, which causes pain and swelling in the joints and connective tissue, accompanied by stiffness particularly in the mornings and when rising from a seat. Most commonly affected sites are the hands, feet, lower back, neck and knees, with movement in these areas becoming severely limited. Chronic fatigue is a common complaint linked with this condition. If you are experiencing mild aches and pains and have psoriasis, even very mildly, consult your dermatologist for further advice and if necessary a referral to a rheumatologist for further assessments. For more detailed information on psoriatic arthritis see What is Psoriatic Arthritis?
You May Like: Light Therapy For Psoriasis At Home