Vitamin D And Inflammation
The relationship between vitamin D and certain cytokines may contribute to PsA and osteoporosis. Together, vitamin D and cytokines help to maintain and regulate the functions of the skin and bones.
Vitamin D deficiency is a known risk factor for osteoporosis and may also be involved in PsA. One study found that chronic inflammation in PsA was also associated with a deficiency of vitamin D, as well as the overproduction of cytokines. Too little vitamin D and too many inflammatory cytokines likely contribute to the loss of bone mineral density and lead to the development of osteoporosis in people with PsA. Experts are uncertain whether vitamin D and cytokines work together or control each others functions.
Common Psoriatic Arthritis Symptoms Include:
Swollen fingers and toes
Tender, painful, or swollen joints
Reduced range of motion of joints
Morning stiffness
Lower back, upper back, or neck pain
General fatigue
or separationfrom nail bed
If you are experiencing any symptoms of psoriatic arthritis listed above, it’s important to talk to your doctor.
You Can Develop Psoriatic Arthritisanytimebefore Or After Your Psoriasis Diagnosis
Medical experts used to believe that people with psoriasis could only develop psoriatic arthritis within 10 years of their initial psoriasis diagnosis, according to the Cleveland Clinic. However, studies have shown that this isnt true. In fact, up to 15% of people with both diseases actually experienced their psoriatic arthritis symptoms first, according to the Cleveland Clinic. Some people may develop psoriatic arthritis before psoriasis, and others may have had psoriasis for years without realizing it, according to Dr. Giangreco. Psoriasis can remain hidden from patients on the back of the scalp or buttock area and go unnoticed for long periods of time, Dr. Giangreco tells SELF. If you have psoriatic arthritis and suddenly notice changes in your skin and nails, then you dont want to rule out the possibility of psoriasis. Rarely do people have psoriatic arthritis without getting psoriasis, too, according to the U.S. National Library of Medicine.
Read Also: Best Natural Shampoo For Psoriasis
Treatments Target Markers In The Blood
Generally, dermatologists treat mild psoriasis in patientswithout PsA with a topical cream or phototherapy that only penetrates the topskin layers.
However, for someone who has PsA and/or moderate to severe psoriasis, pills or injected medications often biologics are needed to control systemic inflammation. There are now many treatment options that effectively control psoriasis inflammation in both the skin and joints.
Topical medications have no way to control systemicinflammation, Dr. Fernandez says. Thats why pills and injectables are soimportant. They can access the bloodstream and can reduce inflammation all overthe body.
While glucocorticoids are a help, injecting them can carry asmall risk of serious joint infection, and side effects make long-term useundesirable. Your doctor will likely screen for active infections or a historyof frequent infections when deciding whether to use this therapy.
Some pills may stimulate liver inflammation. They can alsoreduce blood counts or impair kidney function, he says.
The Importance Of Early Diagnosis In Psoriatic Arthritis
Because PsA is progressive and can cause irreversible joint damage, early diagnosis and treatment are critical. The earlier your condition is identified, the more likely doctors can slow or stop joint damage with medication. Treatment options may include biologics such as etanercept and adalimumab , and disease-modifying antirheumatic drugs such as methotrexate and the newer apremilast .
There are several challenges in diagnosing PsA, including lack of standardized criteria and the wide range of doctors people with this condition might see. If you have symptoms of psoriatic arthritis, you may go to your primary care doctor, dermatologist or rheumatologist. We see a lot of patients coming in with a delayed diagnosis. And now that we have such great treatments to manage the symptoms and slow down progression, we really want to find these patients, says M. Elaine Husni, MD, vice chair of rheumatology at the Cleveland Clinic in Ohio.
Also Check: What Does Psoriasis Scalp Look Like
How Can Psoriatic Arthritis Be Identified Earlier
A number of educational initiatives aimed at bringing together rheumatologists and dermatologists to learn from each other about psoriasis and psoriatic arthritis have been initiated. The good news is its possible to diagnose the majority of PsA patients based on history and a physical exam alone, prior to the results of the lab work and X-rays. Thus dermatologists who may not order lab work or X-rays can still feel confident about identifying patients who need to be referred to rheumatologists.
As a patient, you should be proactive and tell your doctor about any joint symptoms you may be experiencing. These may include joint pain of a noticeable duration , morning stiffness and joints that feel swollen or warm for days at a time.
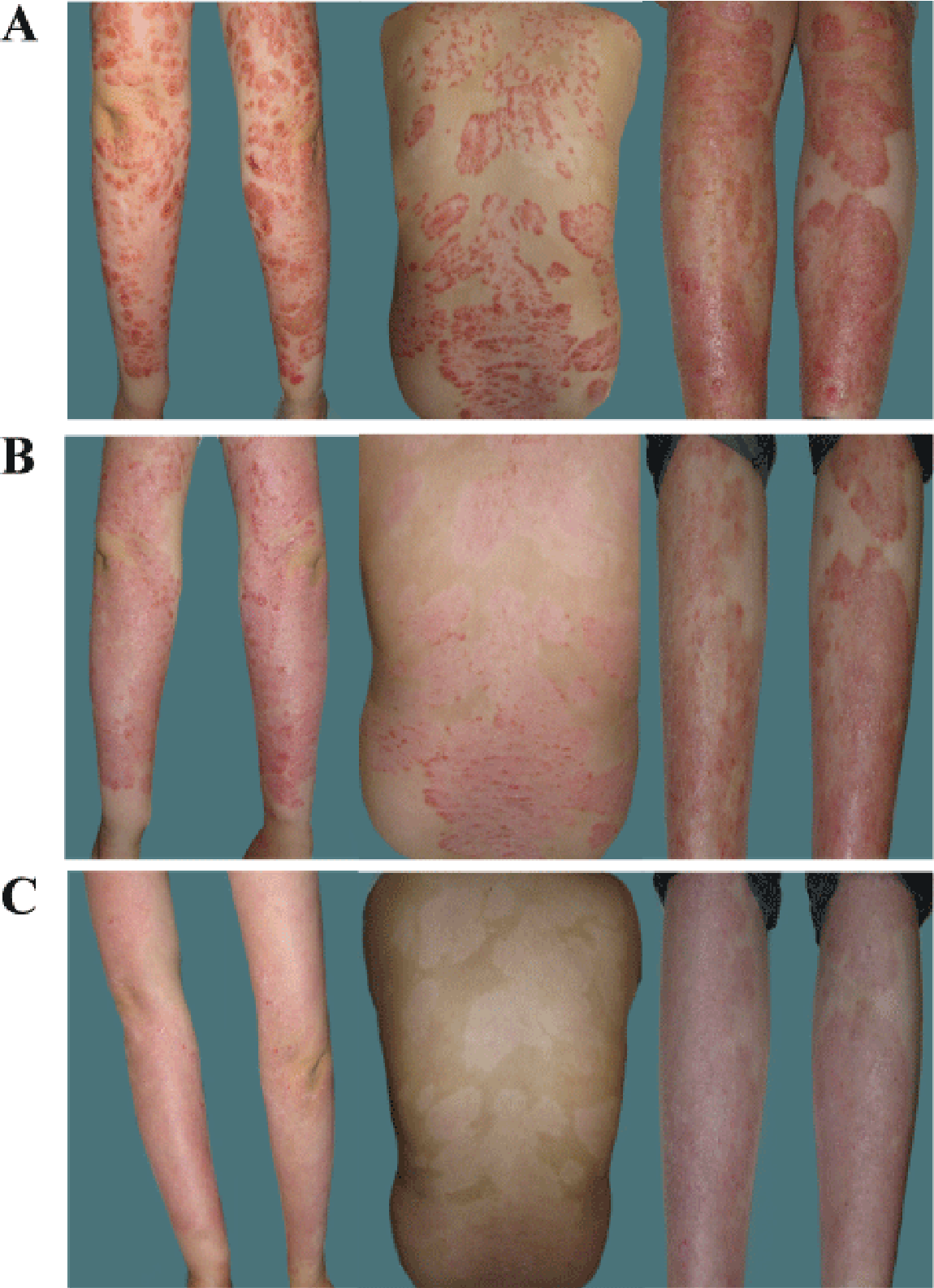
The Effects Of Psoriasis And Psa
The most common form of psoriasis is plaque psoriasis, also known as psoriasis vulgaris. It affects 80 to 90 percent of all people with psoriasis. Its characterized by plaques. These may come and go, even though psoriasis is a chronic, or long-term, disease.
Like psoriasis, PsA is chronic. PsA is also a progressive condition. It gets worse over time. The inflammatory response that PsA triggers in joints can lead to the gradual destruction of joint cartilage and bone.
If left untreated, this process can result in twisted, painful, or swollen joints that no longer function. Joint pain may be widespread or may only occur on one side of your body.
If you have psoriatic disease, youre also at risk for other conditions. This includes:
Also Check: Vitamin D Cream For Psoriasis
What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
There Are Many Treatment Options Available To People With Psoriasis And Psoriatic Arthritis It Can Seem Overwhelming But It Sure Beats Not Having Enough Options
Mild psoriasis is typically treated with creams, ointments, and lotions applied directly to the skin, most often with topical steroids. Mild psoriasis treatments are examined here. Those with moderate or severe psoriasis also sometimes use such topical treatments, particularly for stubborn psoriasis patches or other hard-to-treat areas.
But most moderate to severe psoriasis and psoriatic arthritis is treated with treatments that impact the whole body: ultraviolet lights directed at the skin, pills that are taken by mouth, injections made under the skin, and infusions directly into the bloodstream.
Today patients can select treatments that are more effective, more safe, and able to be used longer than ever before. We review these options below.
Read Also: What Can You Do For Scalp Psoriasis
What Causes Psoriasis And Psoriatic Arthritis
The symptoms of both psoriasis and psoriatic arthritis arise when the bodys immune system malfunctions, leading to inflammation.
In psoriasis, the faulty reaction causes skin cells to grow too fast, promoting a buildup of skin cells on the surface. These cells appear as a scaly rash.
In psoriatic arthritis, the inflammation affects the joints. Permanent damage can result if the person does not seek treatment.
Doctors do not yet know the exact causes of psoriasis and psoriatic arthritis. However, they do know that genetics contribute to both conditions.
An estimated 1 out of 3 people with psoriasis say that they have a family member with psoriasis. Also, around 40 percent of people with psoriatic arthritis have a family member with psoriatic disease.
Still, many people have genes for psoriatic disease and never develop it. To develop psoriatic disease, a person must have the specific genes for it, as well as a trigger that activates it.
Possible triggers for psoriatic disease include:
- an infection, such as strep throat or a cold
- use of tobacco or smoking
- heavy alcohol use
These triggers may bring on psoriasis, and they can also cause flares. Flares are cycles during which symptoms become worse. Triggers vary from person to person and may change over time.
Psoriasis and psoriatic arthritis symptoms often come and go in cycles. They may get worse during a flare and then improve. Symptoms may also move around, affecting different areas of the body at different times.
Who Is At Risk For Psoriatic Arthritis
Psoriasis affects 2-3 percent of the population or approximately 7 million people in the U.S. and up to 30% of these people can develop psoriatic arthritis. Psoriatic arthritis occurs most commonly in adults between the ages of 35 and 55 however, it can develop at any age. Psoriatic arthritis affects men and women equally.
It is possible to develop psoriatic arthritis with only a family history of psoriasis and while less common, psoriatic arthritis can occur before psoriasis appears. Children of parents with psoriasis are three times more likely to have psoriasis and are at greater risk for developing psoriatic arthritis. The most typical age of juvenile onset is 9-11 years of age.
Recommended Reading: How Long Does It Take To Get Rid Of Psoriasis
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Lifestyle Remedies For Psoriatic Arthritis

Making lifestyle changes can prevent and control flares as well as alleviate the muscle weakness and joint stiffness associated with psoriatic arthritis. Lifestyle remedies include the following:
- Use assistive devices during flare-ups. Immobilize certain body parts with the use of splints, braces, orthotics, crutches, or walkers so they can rest.
- Exercise can keep joints flexible, strengthen your muscles, and boost your overall health. Walking, biking, swimming, and yoga are just a few exercises that wont stress your joints.
- Protect your joints by modifying how you perform daily tasks. For example, use a jar opener to remove a lid.
- Apply hot and cold packs. The heat and cold can help lessen the pain sensation.
- Keep your weight at a healthy level. Your joints will have less strain on them as a result.
You May Like: Is Psoriasis Hereditary From Parents
Do We Know What Causes Psoriatic Arthritis
- The cause of psoriatic arthritis is the subject of much research.
- You cannot catch psoriatic arthritis or psoriasis from someone else. Therefore they are not contagious.
- The cause of psoriatic arthritis is not proven but experts believe it to be a combination of genetic, immunological and environmental factors. 2 out of 5 people with psoriasis or psoriatic arthritis have a first-degree relative with the condition. This means you have a higher chance of developing psoriasis or psoriatic arthritis if you have relative who has the condition. Some experts believe infections such as streptococcal infections may provoke psoriatic arthritis, though this is not proven.
- The role of bacteria in the gut and developing psoriatic arthritis is the subject of current research.
- Trauma and stress may be contributing factors, although this is not proven.
- The genetic make-up of an individual is likely to determine the risk of developing psoriasis and psoriatic arthritis and probably influences the severity.
- Being overweight is now understood to be linked to developing psoriatic arthritis and is the subject of ongoing research.
- There are certain genetic markers linked to the immune system which are now being used to predict the severity of psoriatic arthritis. Much more is known about the mechanisms that lead to inflammation in other conditions and it is likely advances in science will lead to much more effective treatments with fewer side effects.
What Are The Risks Of Biosimilars
The risks and side effects of biosimilars are the same as those associated with their biologic reference product. Anyone considering taking a biosimilar should talk with their health care provider about the short- and long-term side effects and risks. It is important to weigh the risks against the benefits.
Biologics and biosimilars act on cytokines, which are specific proteins released by the immune system that can cause inflammation. Biologics suppress the function of the overactive immune system. When on a biologic or biosimilar, you may have a higher risk of infection. If you develop any signs of an infection, contact your health care provider right away.
Signs of infection include:
- Damp, sticky feeling or sweating
- Fever
Read Also: What Is The Best Steroid Cream For Psoriasis
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
How Do Psoriasis And Psa Overlap
For every 10 patients who walk in the door with psoriasis, about three or four of them will eventually get PsA, says Elaine Husni, MD, MPH, vice chair of the department of rheumatic & immunologic diseases at the Cleveland Clinic in Ohio. Most cases almost always start with the skin condition and then within seven to 10 years later, joint pain symptoms start to develop.
However, skin and joint symptoms can develop at the same time and, more rarely, joint symptoms can appear before skin involvement, says Dr. Haberman. While estimates vary, one study showed that up to 3 percent of patients developed joint disease before skin disease, she notes.
In some cases, there may have been skin involvement that went unnoticed or undiagnosed. For example, psoriasis can be sneaky and show up in hidden or private areas like the scalp, intergluteal cleft , belly button, and inside the ear, explains Dr. Husni. Since people dont really examine their scalp or buttocks very often, small psoriasis patches can get missed and delay diagnosis, she says.
Adds Dr. Haberman: You might have a small fleck in your scalp that you just think of as dandruff that is actually psoriasis.
Whats more, people with psoriasis in some of these hidden areas may actually be more prone to PsA. Studies have shown that you may be at higher risk of developing PsA if you have scalp, nail, or inverse psoriasis, says Dr. Haberman.
You May Like: Blue Star Ointment Good For Psoriasis
What Is Psoriatic Arthritis
Psoriatic arthritis is a type of arthritis linked with psoriasis, a chronic skin andnail disease. Psoriasis causes red, scaly rashes and thick, pitted fingernails.Psoriatic arthritis is similar to rheumatoid arthritis in symptoms and jointswelling . But it tends to affect fewer joints than RA. And it does notmake the typical RA antibodies. The arthritis of psoriatic arthritis comes in 5forms:
- Arthritis that affects the small joints in the fingers, toes, or both
- Asymmetrical arthritis of the joints in the hands and feet
- Symmetrical polyarthritis, which is similar to RA
- Arthritis mutilans, a rare type of arthritis that destroys and deforms joints
- Psoriatic spondylitis, arthritis of the lower back and the spine
Psoriasis and Psoriasis Arthritis FAQ
But Is Anyone Ever Really Prepared For A Life
As told to Erica Rimlinger
My grandmother had psoriasis, an auto-immune condition that affects the skin. Although it can be inherited, none of her children have it, none of my 10 cousins have it, and none of my three brothers and sisters have it. But I do.
In fact, I’ve been living with it for such a long time I don’t remember not living with it. But my journey with psoriatic arthritis began just last year. PsA is a form of arthritis that can affect people who have psoriasis, and although it can be controlled, it can’t be cured. It can range from mild to disabling. One year after my PsA diagnosis in 2020, I’m still more or less coming to terms with it, and I’m not yet sure how serious my case will be.
Psoriasis is such a visible disease it’s hard to miss. When I was a child, I only had a few flare-ups and they would start with a couple of small red spots here and there that almost looked like measles or chickenpox.
If you have psoriasis, you have a higher chance of getting PsA, so the fear that I could develop the condition loomed in the back of my mind. I always knew there was a chance I could get it. Knowing that I’ve had psoriasis for such a long time, my doctor would ask at every appointment, “How do your joints feel? Are you having any pain in the morning?” Until last year, the answer was always no.
This resource was created with support from Bristol Myers Squibb
You May Like: How To Treat Psoriasis On Hands