Are There Any Specific Vaccine Side Effects To Be Aware Of With Psoriatic Arthritis
Some COVID-19 vaccine side effects could resemble those of a psoriatic arthritis flare. Its important to carefully track your symptoms and talk to your doctor if you have any concerns. Typically, vaccine side effects only last a few days .
The CDC lists the following common side effects from the COVID-19 vaccine:
- Pain on the arm where you got the shot
- Redness on the arm where you got the shot
- Swelling on the arm where you got the shot
- Tiredness
- Fever
- Nausea
Muscle aches, joint pain, fever, and fatigue can all be common with PsA flares. Nausea can also occur after the vaccine and some PsA patients may experience nausea after taking certain medications like methotrexate.
Some vaccine recipients also reported a delayed skin rash after receiving the Moderna vaccine in its phase 3 clinical trial, per a March 2021 letter to the editor published in the New England Journal of Medicine. The reactions typically resolved over the next four to five days. These types of reactions are not contraindications to getting another vaccine, so all participants were encouraged to finish their vaccine source .
For more information on distinguishing disease flares from vaccine side effects, heres our guide on what to do after getting a COVID-19 vaccine if youre immunocompromised or have an autoimmune condition.
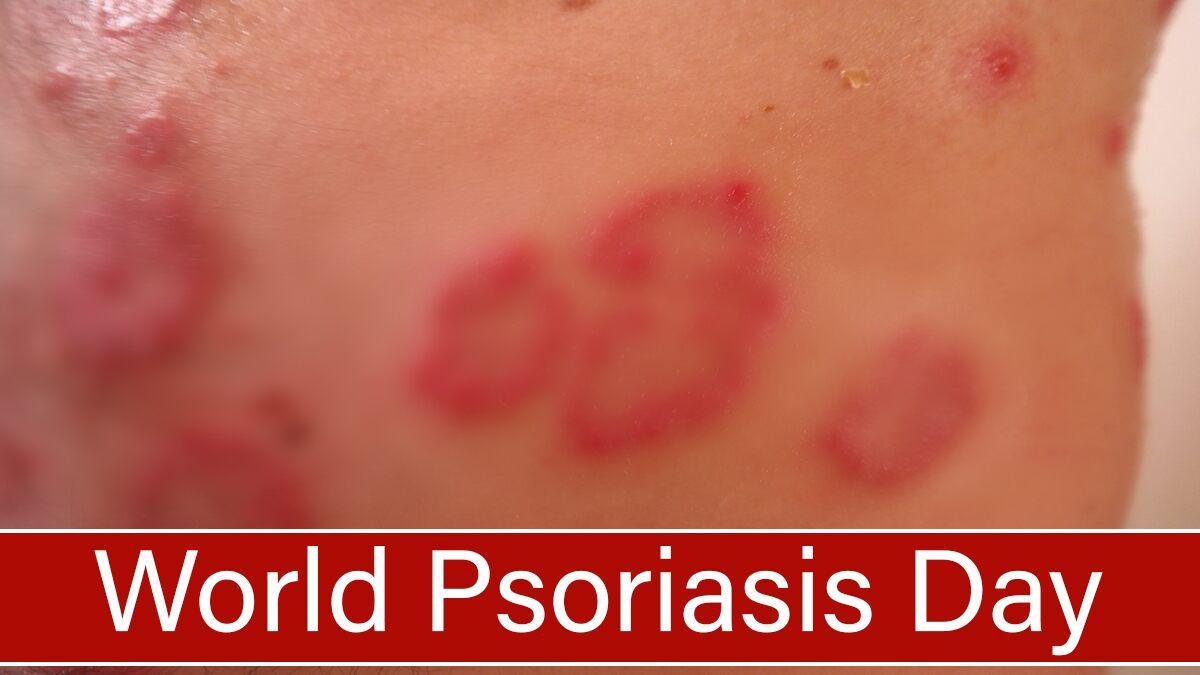
Can Psoriasis Go Away On Its Own
Psoriasis is a skin disease accompanied by symptoms of red, itchy, and patchy skin. In most cases, it needs to undergo treatment while some cases may be associated with spontaneous remission. The flare-up in such skin conditions may disappear or undergo healing on its own and without any treatment.
Probably the spontaneous remission is a result of the immune system which may stop attacking the skin, making the symptoms fade away. Even after getting treated there are chances of reoccurrence.
How Does The Immune System Work
Your immune system is supposed to protect against infection and diseases through inflammation. It does this by sending immune cells and blood to parts of the body it feels are threatened. For example, if you fall and scrape your elbow, it will swell and become red as your immune systems inflammatory response works to heal the injury.
The immune system works with both your circulatory and lymphatic systems. This involves the transportation of antigens and pathogens to lymph nodes and/or the spleen for processing and eradication. Immune cells, including phagocytes and neutrophils, circulate through the circulatory system to the location of the pathogenseither in the lymph nodes or spleento overwhelm and destroy foreign invaders.
The immune system works to eradicate pathogens with help from the integumentary system. The integumentary system is made up of all the skin cells of the body. Both the skin and the immune system work together to keep foreign pathogens out of the body. Interestingly, the skin is the first line of defense because it acts as a barrier to the inner body.
Read Also: Does Lemon Juice Help Psoriasis
Genetic Background Of Psoriasis And Its Relationship To Immune Function
Investigators have long appreciated the genetic nature of psoriasis. The concordance rate of psoriasis is approximately 70% in monogenic twins and 20% in dizygotic twins, depending on the study and the population . Approximately three billion base pairs exist in the human genome, and only 35% of these sequences code for proteins. A disease-causing mutation is usually quite rare and is commonly found in a coding or regulatory region. Psoriasis is a complex disease with over 30 single nucleotide polymorphisms contributing to disease risk, but two gene mutations have recently been found that can independently induce psoriasis , and these genes have an effect on both the skin and the immune system.
What Are Autoimmune Diseases

Your immune system is made up of organs and cells meant to protect your body from bacteria, parasites, viruses and cancer cells. An autoimmune disease is the result of the immune system accidentally attacking your body instead of protecting it. It’s unclear why your immune system does this.
There are over 100 known autoimmune diseases. Common ones include lupus, rheumatoid arthritis, Crohns disease and ulcerative colitis.
Autoimmune diseases can affect many types of tissues and nearly any organ in your body. They may cause a variety of symptoms including pain, tiredness , rashes, nausea, headaches, dizziness and more. Specific symptoms depend on the exact disease.
Don’t Miss: Can You Develop Psoriasis In Your 60s
There Are Ways To Shorten Flare
Psoriasis is a big star on TV drug ads, but this autoimmune skin disease is something most people try to keep well hidden.
“Psoriasis is among the most common skin conditions, affecting about 2% of the U.S. population, and while the condition doesn’t affect everyone the same way, the approach to treatment and prevention is often similar,” says Dr. Gideon Smith, an assistant professor of dermatology at Harvard-affiliated Massachusetts General Hospital.
More Than Skin Troubles
A 2017 study from the Journal of the American Academy of Dermatology found that people with psoriasis that covers 10% of their body or more are 64% more likely than those without psoriasis to develop type 2 diabetes. “About 30% of people with psoriasis also might develop psoriatic arthritis, which causes destructive inflammation in your joints,” says dermatologist Dr. Gideon Smith. Psoriasis also may signal a higher risk for fatty liver disease and heart attacks.
Also Check: Ways To Treat Psoriasis At Home
How To Prevent Psoriasis
Psoriasis is a skin disease and one should consult with a dermatologist for its treatment. However, there are some home remedies that can prove to be effective for the prevention and management of the condition. Some of those remedies include:
- Regular application of moisturizing lotions on the skin so as to prevent the skin from drying.
- Proper care for the skin and scalp should be taken which includes the use of medicated shampoos on the scalp and regular bathing with medicated products.
- Exposure to cold as well as dry weather should be avoided, humidifiers may be used inside the house.
- Prescribed medicines should be preferred.
- Stress should be avoided.
What Are Other Types Of Psoriasis
Plaque psoriasis is the most common type. About 80% to 90% of people with psoriasis have plaque psoriasis.
Other, less common types of psoriasis include:
- Inverse psoriasis appears in skin folds. It may look like thin pink plaques without scale.
- Guttate psoriasis may appear after a sore throat caused by a streptococcal infection. It looks like small, red, drop-shaped scaly spots in children and young adults.
- Pustular psoriasis has small, pus-filled bumps on top of the red patches or plaques.
- Sebopsoriasis typically appears on the face and scalp as red bumps and plaques with greasy yellow scale. This type is a cross between psoriasis and seborrheic dermatitis.
Read Also: How Can I Get Rid Of Psoriasis Fast
How Long Does It Take To Recover
The recovery period depends on your skin type and the nature of the treatment used. For some individuals, the results can be immediate, whereas for some individuals the effect can take some time. The doctor would initially check how well you are responding to the treatment and make some changes if the desired results are not got.
Myeloid Dendritic Cells In Healthy Skin
A resident population of DCs in the dermis also contributes to the ability of skin DCs to activate T cells after encountering antigens. In the late 1980s, dermal immune cells were first characterized using a marker to the clotting factor Factor XIIIa . FXIIIA+ cells were large, fluffy cells with dendritic morphology scattered throughout the dermis, and they were called dermal DCs or dermal dendrocytes. However, in recent years, newer antibodies identifying these dendritic dermal cell populations have become available, including the x integrin CD11c, which identifies interstitial DCs . When healthy dermis was stained with CD11c, a different pattern of positive cells was observed in the upper dermis, which contrasted with the FXIIIA+ cells scattered throughout the dermis . Two-color immunofluorescence showed that CD11c and FXIIIA indeed identified two distinct populations of cells.
You May Like: Homeopathic Treatment For Psoriasis On The Scalp
Most Common Autoimmune Diseases
1. Rheumatoid Arthritis Rheumatoid arthritis is a chronic inflammation of the lining of the joints, leading to pain and swelling typically in the hands and feet. It can affect anyone, but is most prevalent in women over 40. Rheumatoid arthritis can sometimes affect other organs as well, such as skin, eyes, lungs and blood vessels. As with all autoimmune disorders, treatment focuses on managing pain and minimizing bone erosion and joint damage.
We have more in-depth information on Rheumatoid Arthritis here.
2. Juvenile Rheumatoid Arthritis Juvenile rheumatoid arthritis is the most common form of arthritis in children under 16. Symptoms usually include pain and swelling in the joints, and can vary from moderate to severe. In some cases, symptoms will subside over time while others can persist well into adulthood.
We have more in-depth information on juvenile rheumatoid arthritis here.
3. Systemic Lupus Erythematosus Lupus can be difficult to diagnose because it shares symptoms with many other disorders. The inflammation resulting from lupus can affect many different areas of the body, from the lungs, heart, joints, skin, kidneys, and brain. Like rheumatoid arthritis, lupus is more prevalent in women and can sometimes be identified by a butterfly-shaped rash on the face, along with photosensitivity, fatigue and fever, joint pain, and other skin lesions that worsen under sun exposure.
We have more in-depth information on lupus here.
Need For An Integrated Multidisciplinary Care Of The Psoriatic Patient
Research and models focused on the pathogenesis of psoriasis as a systemic immune-mediated inflammatory disease should not remain speculative and self-referential, rather they should lead to a more coherent and comprehensive model of the clinical approach to the psoriatic patient. Research groups, such as the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis , now emphasize the concept of psoriatic disease rather than psoriasis . An integrated approach to the psoriatic patient is needed today, which has been shown by various studies to improve patient care .
The management of the psoriatic patient today raises strictly practical problems in daily clinical practice. Pre-therapeutic check-ups before starting biological or systemic therapies, which usually consist of instrumental and routine laboratory tests, sometimes lead to detection of abnormalities requiring specialized extra-dermatological evaluation. Moreover, the multidisciplinary approach to psoriasis usually leads to finding the most appropriate treatment for any specific patient.
For example, in psoriatic arthritis, nonsteroidal anti-inflammatory drugs are effective in improving joint symptoms, especially in case of the mild disease. However, in case of even mild skin involvement, early treatment with conventional synthetic disease-modifying anti-rheumatic drugs should be considered .
Don’t Miss: How Many People Have Plaque Psoriasis
Having Psoriasis During The Covid
Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
This has been reviewed and updated as of May 29, 2020.
Because psoriasis primarily impacts the skin, many people assume it is merely a cosmetic problem. In reality, psoriasis is an autoimmune disease. This means that an overactive immune system is driving inflammation and overproduction of skin cells.
As with other autoimmune conditions, psoriasis patients may have a higher than average risk of contracting COVID-19 or developing serious complications, though more research on this patient population is needed. It is too preliminary to say whether or to what degree people with psoriasis could be affected differently by COVID-19.
An observational study that aims to determine how prevalent COVID-19 is in psoriasis patients who are using immunosuppressive medication is currently underway in Italy.
Recently, a study from the Perelman School of Medicine at the University of Pennsylvania found that psoriasis patients who use an IL-17 inhibitor were more likely to develop respiratory tract infections during previously conducted drug trials. They did not specifically look at risk for COVID-19, as these trials were conducted prior to the pandemic.
The flip side: IL-17 inhibitors have shown some promise as a potential treatment for COVID-19 patients who experience a cytokine storm.
Heres what you can do to stay healthy.
How Does Psoriatic Disease Affect The Immune System
Psoriatic disease is an immune-mediated disease that includes psoriasis, along with other comorbidities such as psoriatic arthritis and related systemic inflammation. In people living with psoriasis and/or PsA, the immune system is triggered and activated, acting as though there are harmful pathogens attacking the body.
This inflammation can present with noticeable signs such as discoloration of the skin or swelling around joints. However, the overactive immune system may also lead to inflammation a person cannot see. It can affect in the body, organs and systems and lead to other health conditions associated with psoriatic disease. Comorbidities of psoriatic disease include cardiovascular disease, metabolic syndrome, obesity, hypertension , type 2 diabetes, anxiety and depression, and more.
Researchers who study psoriatic disease are still working to identify the substances inside the body that trigger this immune response. One possibility could be certain kinds of bacteria acting as antigens . For example, sometimes streptococcal infection can trigger a case of guttate psoriasis. Another possible antigen could be antimicrobial peptides, molecules made by the body that are a part of the immune system and that work as antibiotics. *
Recommended Reading: What Helps Psoriasis On Face
How To Get The Right Arthritis Diagnosis
There is no single test for psoriatic arthritis, says Azar. Along with a physical exam, youll likely need a series of both imaging procedures and blood tests for a diagnosis, and to rule out other forms of arthritis, such as rheumatoid arthritis or gout.
Theres no one test to diagnose rheumatoid arthritis either, but, as with PsA, blood tests are part of the workup. The presence of autoantibodies in the bloodstream, either rheumatoid factor or cyclic citrullinated peptide antibodies, will suggest an RA diagnosis. These antibodies tend to be less typical in people with psoriatic arthritis, according to an article published in Rheumatic and Musculoskeletal Diseases in August 2018.
As part of the physical exam, the doctor will closely evaluate the affected joints. RA involves the joints in a symmetrical fashion, and often, when rheumatoid factor is very high, there may be nodules under the skin, Azar says. According to the National Rheumatoid Arthritis Society, 20 percent of patients with RA develop these firm lumps.
Psoriatic arthritis, on the other hand, can reveal itself in a variety of ways, affecting a large joint or a single small finger joint of the hand, says Azar.
Another notable difference between the two diseases is bone involvement. RA is characterized by bone loss or erosion near the joint, while PsA is marked by both bone erosion and new bone formation, Azar says. An X-ray or other imaging method can help reveal whats going on.
Signs And Symptoms Of Autoimmune Disease
Autoimmune diseases can develop from a variety of factors with no known definitive causes for the onset of the disease. Some suspected sources are:
- Bacterial or viral infection
- Chemical toxins
- Environmental pollutants
When the immune system determines that healthy cells are foreign, it begins to produce antibodies to fight off the healthy cells it believes to be the source of an illness or infection. When an autoimmune disease is suspected, a rheumatologist will administer tests to determine what antibodies are being produced. There are more than 80 potential autoimmune diseases and some of the most common areas affect can be:
- Joints and muscles
- Blood vessels
- Connective tissue
When faced with symptoms or an autoimmune disease diagnosis, it is very important to seek treatment from an experienced rheumatologist to find the best plan to manage symptoms. Dr. Susan Baker, MD specializes in Rheumatology and Internal Medicine in Beverly Hills, and offers patients everything from arthritis treatment to Lupus.
Also Check: Cimzia Dosing For Plaque Psoriasis
What Else Should I Ask My Healthcare Provider
If you have psoriasis, ask your healthcare provider:
- How can I prevent outbreaks and control symptoms?
- What medication will work best for me?
- What else should I do to improve symptoms?
- What are my options if creams dont work?
- Will psoriasis ever go away?
A note from Cleveland Clinic
Psoriasis, an itchy skin condition, can come and go throughout your life. Its related to an overactive immune response and is not contagious. If you have skin changes that arent going away, talk to your healthcare provider. There is no cure for psoriasis, but psoriasis treatments can improve symptoms. Your provider may prescribe a special cream or moisturizer or medications. Other therapies are available if creams or medicines dont work. Maintaining your overall health will also help improve symptoms.
Last reviewed by a Cleveland Clinic medical professional on 10/17/2020.
References
What Is Cdc Doing About Psoriasis
In 2010, CDC worked with experts in psoriasis, psoriatic arthritis, and public health to develop a public health perspective that considers how these conditions affect the entire population. The resulting report is Developing and Addressing the Public Health Agenda for Psoriasis and Psoriatic Arthritis pdf icon. You can read a short article about the agendaexternal icon in The American Journal of Preventive Medicine.
CDCs National Health and Nutrition Examination Survey , an intermittent source of national psoriasis data, has included questions about psoriasis as late as the 2013-2014 cycle. A recent analysis of NHANES data estimates that 7.4 million adults had psoriasis in 2013external icon.
- Psoriasis causes patches of thick red skin and silvery scales. Patches are typically found on the elbows, knees, scalp, lower back, face, palms, and soles of feet, but can affect other places . The most common type of psoriasis is called plaque psoriasis.
- Psoriatic arthritis is an inflammatory type of arthritis that eventually occurs in 10% to 20% of people with psoriasis. It is different from more common types of arthritis and is thought to be related to the underlying problem of psoriasis.
- Psoriasis and psoriatic arthritis are sometimes considered together as psoriatic disease.
Who is at risk for psoriasis?
Anyone can get psoriasis. It occurs mostly in adults, but children can also get it. Men and women seem to have equal risk.
Can I get psoriasis from someone who has it?
Also Check: Treating Scalp Psoriasis And Seborrheic Dermatitis